Dr Calum Bain
My research focuses on understanding the signals that dictate macrophage behaviour in the healthy tissues and during successful tissue repair so that these signals can be promoted or targeted when macrophages begin to behave abnormally in inflammatory/fibrotic disease.
Dr Calum C Bain
Sir Henry Dale Fellow

- Centre for Inflammation Research
Contact details
- Work: +44 (0)131 242 6654
- Email: calum.bain@ed.ac.uk
- Web: Academic Profile
Group Members
- Wouter T'Jonck - Postdoctoral Research Fellow (UKRI (MCSA-replacement) funded)
- Gareth-Rhys Jones - Wellcome Trust Clinical Career Development Fellow
- Lizi Hegarty – Postdoctoral Research Fellow (UKRI-MRC Trust funded) – joint with Emmerson lab
- Claire Adams - PhD student (Wellcome Trust ECAT)
- Broc Drury – PhD student (EASTBIO programme)
- Sam Bankole – PhD student (EASTBIO programme) – joint with Mabbott lab
Background
All tissues of the body are populated with a mixture of immune cells that help protect the body from invasion by microbes. In many tissues the most abundant immune cell is the macrophage. Macrophages are essential ‘house keepers’, clearing millions of dead cells from the body each day and producing factors to maintain the structural cells of tissues. However, macrophages also orchestrate the inflammation and tissue repair processes during and following injury or infection. However, in some people macrophages can become dysregulated leading to them becoming excessively pro-inflammatory and drive chronic inflammation, such as inflammatory bowel disease (IBD). In other settings, the wound repair functions of macrophages overshoot leading to excessive repair, unconstrained scar formation (fibrosis) and organ dysfunction. For instance, idiopathic pulmonary fibrosis (IPF) is an incurable, devastating, deadly disease where progressive scarring of the lung is believed to involve macrophages with overactive and aberrant behaviour.
Importantly, macrophages are very flexible cells and are easily influenced by their environment, therefore holding great promise as therapeutic targets. Thus, our work focusses on understanding the local environmental cues that determine macrophage identity and function in the healthy tissues and how these change during disease, which will be vital for designing novel macrophage-targeted therapies for disease.
Research Overview
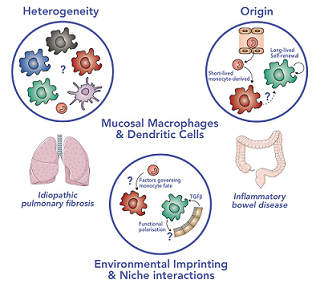
My lab uses a combination of multi-parameter flow cytometry, transcriptional profiling (bulk and single cell RNAseq) and a range of functional assays to determine the heterogeneity and function of mucosal macrophage subsets during health and disease. We use a variety of transgenic mouse models to track monocyte/macrophage dynamics during health, inflammation and tissue repair, and determine the environmental factors that regulate their function. My lab forms an integral part of the Gut Research Unit and has an established pipeline for the collection and analysis of human tissue from IBD patients.
The following PDF provides a brief visual summary of this group’s current research.
The following PDF provides a brief visual summary of this group’s current research.
Biographical Profile
I graduated from the University of Glasgow with a BSc in Immunology in 2007. I was then awarded an MRC PhD studentship from the University of Glasgow and worked with Professor Allan Mowat in the Centre for Immunobiology to investigate the role of macrophages in intestinal homeostasis and disease, for which I was awarded the Joseph Black Medal and Alan Hird Prize in Medicine for the top PhD thesis in the School of Medicine. After completing my PhD in 2012, I continued to work in the Mowat group, where I led their Wellcome Trust funded studies exploring the origin of intestinal macrophages. Collectively, my work demonstrated for the first time that unlike most tissue macrophages, those in the gut wall require constant replenishment by circulating monocytes, in a process that is, in part, dependent on the microbiota. In June 2014 I moved to work with Dr Stephen Jenkins at the Centre for Inflammation Research (CIR) at the University of Edinburgh to take advantage of the plethora of tools available for macrophage research and in vivo fate mapping of myeloid cells. In February 2017, I was awarded a Sir Henry Dale Fellowship from the Wellcome Trust/Royal Society to establish my own lab within the CIR.
Recent publications
The transcription factor EGR2 is indispensable for tissue-specific imprinting of alveolar macrophages in health and tissue repair
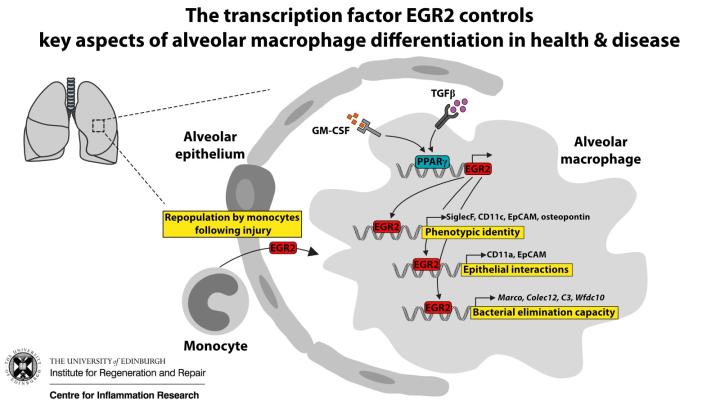
Access full paper at Science.Org website
Honours and Awards
- Joseph Black Medal and Alan Hird Prize in Medicine from the University of Glasgow (2012). This medal is awarded annually for the top PhD thesis in the School of Medicine.
- British Society of Immunology Postdoctoral Bright Sparks in Immunology 2013, an annual competition for postdoctoral scientists based on oral presentations.
- Winner of a Poster Prize at the BSI Congress 2016.
- Wellcome Trust/Royal Society Sir Henry Dale Fellowship.
Public Engagement
- Member and former Chair of Science Festivals subcommittee of the CIR public engagement team.
Other Responsibilities
- Founding member of 'Macrophages@EdUni' interest group
- Co-organiser of the annual 'A cell for all seasons: Macrophages in health and disease' symposium
Collaborators
Internal
- Professor Moira Whyte, CIR - Fellowship sponsor
- Professor Jeffrey Pollard, Centre for Reproductive Health
- Dr Gwo-tzer Ho, CIR
- Professor David Dockrell, CIR
- Professor Philippa Saunders, CIR
- Dr Elaine Emmerson, Centre for Regenerative Medicine
- Dr Rebecca Gentek, CIR
- Dr Doug Gibson, CIR
- Professor Jurgen Schwarze, CIR
External
- Professor Bernard Malissen and Dr Sandrine Henri, CIML, Marseille, France
- Professor Martin Guilliams, VIB, Ghent, Belgium
Funding
More information on funding at Calum's Research Explorer profile

