Dr Laura McCulloch
My research is focused on the effects of stroke on systemic immune function and how this contributes to complications of stroke recovery, including infection, gastrointestinal dysfunction and fatigue.
Dr Laura McCulloch
Sir Henry Dale Research Fellow

- Centre for Inflammation Research
Contact details
- Work: (+44) 0131 242 6552
- Email: laura.mcculloch@ed.ac.uk
- Web: Academic Profile
Group Members
- Dr Isobel Mouat, Post-doctoral Research Fellow
- Rachel Martin, PhD student
Background
An increasing number of stroke patients are surviving long-term after stroke. Complications that effect recovery from stroke (including infection, gastro-intestinal dysfunction, fatigue and cognitive impairments) have rapidly become an area of unmet clinical need. Stroke induces alterations to the systemic immune system which may contribute to these issues and compromise recovery. By understanding the immunological mechanisms that lead to complications of recovery from stroke, we hope to find new therapeutic targets to reduce the impact/ incidence of these complications and improve outcome in stroke patients.

Infection is a common and serious complication of stroke recovery. We have identified deficits in innate-like B cells and circulating IgM antibody due to activation of the sympathetic nervous system and increased production of catecholamines after experimental stroke. This may have an important role in increasing infections in stroke patients and we are investigating whether therapeutic targeting of this pathway may help to reduce this.
Infections occurring at later time points after stroke are also associated with increased death and disability [2]. Considering the danger of infection in both the acute and chronic phases of stroke recovery, little is known of the persistence of the changes to the immune system that occur acutely after stroke or how long stroke patients remain at increased risk of infection.
- Patel, A., et al., Executive summary Part 2: Burden of Stroke in the next 20 years and potential returns from increased spending on research, S. Association, Editor. 2017.
- Learoyd, A.E., et al., Infections Up to 76 Days After Stroke Increase Disability and Death. Translational Stroke Research, 2017.
Research Overview
My research uses integrated experimental animal and clinical studies, clinically relevant models of infection and vaccination, and epidemiological population health data analyses to understand the effect of stroke on the immune system and the immunological mechanisms that underpin complications of stroke recovery, such as increased infection risk. Identifying the underlying immunological mechanisms that result in complications of stroke recovery could provide new therapeutic strategies to reduce these complications and improve outcome and long-term survival after stroke.
The following PDF provides a brief visual summary of this group’s current research.
You can view a full catalogue of graphical research summaries for each group in the Centre for Inflammation Research by visiting our Research page.
Biographical Profile
I obtained my undergraduate honours degree in Immunology from the University of Glasgow. I then carried out my PhD research at the Roslin Institute under the supervision of Prof Neil Mabbott. During my PhD I identified follicular dendritic cells as the key immune cell responsible for replicating prions in peripheral lymphoid tissue to allow subsequent neuroinvasion and CNS disease.
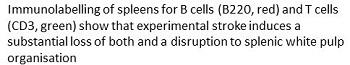
I moved into the field of stroke research as a post-doc working for Dr Barry McColl where we showed that systemic B cell-mediated immune function was compromised after stroke and contributed to acute post-stroke infection susceptibility. We then continued this work at the UK Dementia Research Institute in Edinburgh, and with collaborators at the University of Manchester and Salford Royal, investigating the effects of stroke on B cells in patients and also trialling B cell targeted strategies to reduce infection after experimental stroke.
In April 2021 I started my new position on a Sir Henry Dale fellowship from the Wellcome Trust and Royal Society to start my own research group, continuing my work on post-stroke changes to systemic immune function and strategies to improve outcome after stroke.
Other Responsibilities
Co-chair of the Edinburgh Immunology Group (regional British Society for Immunology affinity group)
Collaborators
- Dr Graeme Cowan https://www.research.ed.ac.uk/en/persons/graeme-cowan
- Dr Calum Bain https://www.research.ed.ac.uk/en/persons/calum-bain
- Dr Barry McColl https://www.ed.ac.uk/discovery-brain-sciences/our-staff/research-groups/dr-barry-mccoll
- Dr Cecile Benezech Cécile Bénézeh | The University of Edinburgh
- Prof Stuart Allan, University of Manchester https://www.research.manchester.ac.uk/portal/en/researchers/stuart-allan(e0dd0cf7-cd2d-4ae1-a6aa-c3781e535276).html
- Prof Craig Smith, University of Manchester and Salford Royal Hospital, NHS Foundation Trust https://www.research.manchester.ac.uk/portal/craig.smith-2.html
- Prof Marion Buckwalter, Stanford University, Marion S. Buckwalter, MD, PhD's Profile | Stanford Profiles
- Dr Zahraa Al Ahmady, Nottingham Trent University, Zahraa Al-Ahmady | Nottingham Trent University
Funding
- Wellcome Trust
- Royal Society
Information on funding at Laura McCulloch's Research Explorer profile.

