Preventing Pesticide Suicide in SE Asia
The Centre for Pesticide Suicide Prevention (CPSP) is a philanthropically funded research and policy initiative within the University of Edinburgh, working to reduce the number of pesticide suicides worldwide.

CPSP aims to identify lethal pesticides responsible for deaths and end their use through regulatory action. It works in low and middle-income countries, where pesticide self-poisoning is a recognised and significant health problem, in collaboration with national policymakers.
The Centre for Pesticide Suicide Prevention: Who we are, What we do (2020)
A global health problem: knowing the facts
An estimated 150,000 people die from pesticide consumption every year, making it one of the most common methods of suicide worldwide.
This is a particular problem in farming communities in South and East Asia, where people have easy access to lethal pesticides which are sold locally without controls and stored in their homes.
The act of self-harm is most commonly spontaneous, and the majority of people do not intend to die. However, the high toxicity of some pesticides means that just one sip can be enough to kill them.
Since the Green Revolution, it is estimated that 14 to 16 million people worldwide have died from ingesting pesticides.
The Centre for Pesticide Suicide Prevention (CPSP) is the first organisation to focus solely on this problem. It works to reduce the number of pesticide suicides occurring worldwide, with the aim of saving hundreds of thousands of lives.
Recognising the issue
“There was no one working on this”
CPSP has grown out of the work of Professor Michael Eddleston, who has worked on pesticide suicides for more than twenty years, particularly in Sri Lanka.
A clinical toxicologist by profession, Michael first became aware of the issue as a student on summer placement in a Sri Lankan hospital. He had been taken on to study snake bites but was alarmed by the number of patients being admitted as a result of pesticide self-poisoning.
“I ended up standing on the medical wards and just watching, seeing what was coming through the doors. I realised that patient after patient was coming in with pesticide poisoning. That is what started me off, seeing these patients and realising that there was no one working on this.”
Michael began working with colleagues in Sri Lanka, including researchers, clinicians and policymakers, supporting their work to identify lethal pesticides and introduce new bans.
Sri Lanka’s regulations have contributed to one of the greatest falls in suicide rates ever seen in the world, with an estimated 93,000 lives saved by 2015.
At the Future Policy Awards 2021, often referred to as the ‘Oscar on best policies’, Sri Lanka was awarded a special accolade in recognition of its policies to regulate highly hazardous pesticides (HHPs).
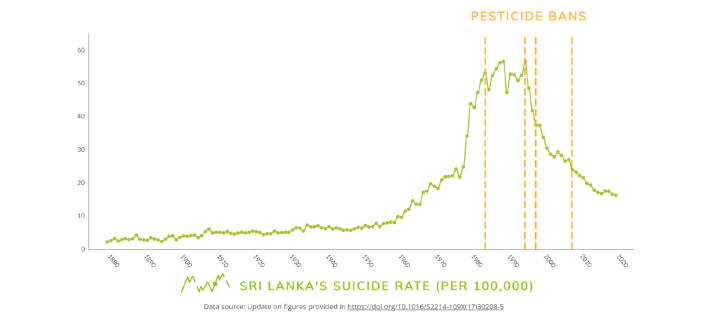
Sri Lanka's success made it clear to Michael that regulation was by far the most effective means of preventing deaths from pesticide poisoning. He saw a need for an organisation that focused on identifying problematic pesticides and supporting effective pesticide regulation globally.
In 2017, the Centre was launched with support from an Incubator Grant of the Open Philanthropy Project Fund, on the recommendation of GiveWell.
Restricting lethal means: how CPSP operates
CPSP’s approach is based on the principal of restricting lethal means – limiting access to lethal pesticides responsible for suicides.
After first finding out what is known about pesticide poisoning in a country, CPSP supports local researchers to collect further, necessary data. It works closely with the health sector, police and other authorities within each country. This information is then passed on to local regulators, helping them to implement reforms that suit their needs, including phasing out or banning the most lethal pesticides.
The Centre also works with health and agricultural officers within countries to measure the impact of the bans on suicide rates and agriculture, ensuring that as lives are being saved, crop production is not being negatively affected.
Nepal: a notable success
With the centre’s formation, the team were able to expand their work to other countries throughout Asia. One notable success has been their work in Nepal.
Nepal is a country that is heavily dependent on agriculture, where pesticides are widely used and are easily accessible within communities. In 2018–19, Nepal recorded 5,754 suicides – a high number for a relatively small country. Over 24% of these suicides were by poisoning, most by ingestion of highly concentrated agricultural pesticides. In 2019, a CPSP study, and subsequent discussions with Nepalese policy makers, resulted in a national ban on a number of pesticides.
“In part due to these conversations [with CPSP], the Pesticide board took the decision in February 2019 to ban 5 highly hazardous pesticides, including dichlorvos, from agricultural use. These represent all the WHO Class II, IB pesticides that were still being used in Nepal. We believe that these bans will reduce suicides and episodes of severe occupational poisoning in the country.”
CPSP is now monitoring the impact of these bans on suicide rates.

India: ongoing work in two states
Pesticide self-poisoning is the second most common method of suicide in India, making it an important focus of CPSP’s work in South Asia. While the official number of self-poisoning deaths are estimated to be 25,764 per year, multiple studies show that the actual number could be up to 50,000.
Given the challenge of working in a country with a large population, CPSP has started its work in two states – Maharashtra and Tamil Nadu. It hopes this work will lead to other states, and eventually the central government, bringing in more measures to prevent pesticide suicides.
This work is being coordinated by colleagues based at the University of Edinburgh India Liaison Office in Mumbai.
Read more on the ongoing work in India here.
Maharashtra
Maharashtra has the highest number of suicides in India and is also one of the largest consumers of chemical pesticides in India. In 2019, CPSP signed a Memorandum of Understanding with the Medical Education and Drugs Department, Government of Maharashtra and began collecting data on pesticide poisoning deaths.
By studying forensic data, CPSP researchers have been able to examine specific compounds responsible for pesticide poisoning cases. Further analysis has allowed researchers to make projections on how the removal of highly hazardous pesticides (HHPs) could affect suicide rates. These projections suggest that bans on HHPS can significantly reduce the number of deaths in Maharashtra.
CPSP’s next steps are to work with the state to help it become one of the first in India to implement pesticide poisoning treatment and control protocols. The Centre also hopes to work with local stakeholders and other relevant government departments such as Agriculture, Public Health, Chemicals and Fertilizers that can guide policy decisions surrounding safe pesticide usage in the state.

Tamil Nadu
Tamil Nadu accounts for the second-highest suicide deaths in the country. The National Crime and Records Bureau recorded 16,883 suicide deaths in 2020 - 12% of total official number of suicide deaths in India – with a quarter of these a result of pesticide self-poisoning. However, under-reporting means that the number may be far higher. There is also the added burden of accidental poisoning cases.
CPSP is currently working closely with both the health and agriculture departments to support the development of legislation that will withdraw six lethal pesticides and one rodenticide from use. A draft bill has already been drafted and presented to the state chief secretary.
Successful regulation of HHPs is recognised to offer clear public health benefits for the state. CPSP’s work in other countries has yielded marked success; the work in Tamil Nadu offers a positive example for other states in India.
“Our work with the Tamil Nadu government is very significant because the state is singularly focused on banning pesticides as a suicide prevention strategy, instead of working on pesticide regulation as a purely agro-economical issue with suicide prevention as a side-effect.”
There has already been some success, with a ban on one rodenticide introduced earlier this year. With CPSP’s support, the state has also taken steps to improve data collection and recording of suicides and poisonings. This will help them make a more informed decision in the future.
What next?
In 2021, CPSP received further Open Philanthropy funding to continue and develop its work. The team has grown significantly, with twenty colleagues now based across four different continents.
While its work in Asia remains a key focus, new partnerships have allowed it to expand into other regions, including Africa and the Caribbean.
The centre is also developing relationships with regional groupings of national pesticide regulators, including the Asia Pacific Plant Protection Commission (APPPC), to strengthen regional capacity and collaboration on the identification, reporting, regulation, replacement and monitoring of highly toxic pesticides.
Meanwhile, CPSP’s work will soon be complemented by a new NIHR Centre at the University of Edinburgh – the Centre for Acute LMIC (low and middle-income countries) Poisoning - which aims to improve the care of acutely poisoned patients. The new centre, also led by Professor Michael Eddleston, will focus on unintentional poisoning, including occupational pesticide poisoning.
CPSP's work in collaboration with national policymakers and global partners has already changed clinical practice and led directly to pesticide regulation across Asia. This has prevented and will continue to prevent, many thousands of deaths from pesticide poisoning.
Read more about the Centre for Pesticide Suicide Prevention
Find more information on their webpages at www.centrepsp.org

