New Study Sheds Light on the Impact of Blood Pressure Lowering Medications on Brain Health
Hypertension, or high blood pressure, is a leading risk factor for cerebral small vessel disease, a condition that affects the small blood vessels in the brain and which causes stroke and dementia.
Recent research from a multicentre, open-label, randomised crossover trial conducted at five specialist centres in Europe funded by the Horizon 2020 programme, has examined the impact of different antihypertensive drug classes on small blood vessel function in people with small vessel disease.
Lead by researchers at the Ludwig Maximilian University of Munich and the University of Edinburgh’s Row Fogo Centre for Research into Ageing and the Brain, the TREAT-SVDs study included participants with symptomatic sporadic small vessel disease or cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). The research team aimed to determine whether specific antihypertensive medications yielded differing effects on cerebrovascular reactivity (CVR), an important indicator of brain blood vessel health.
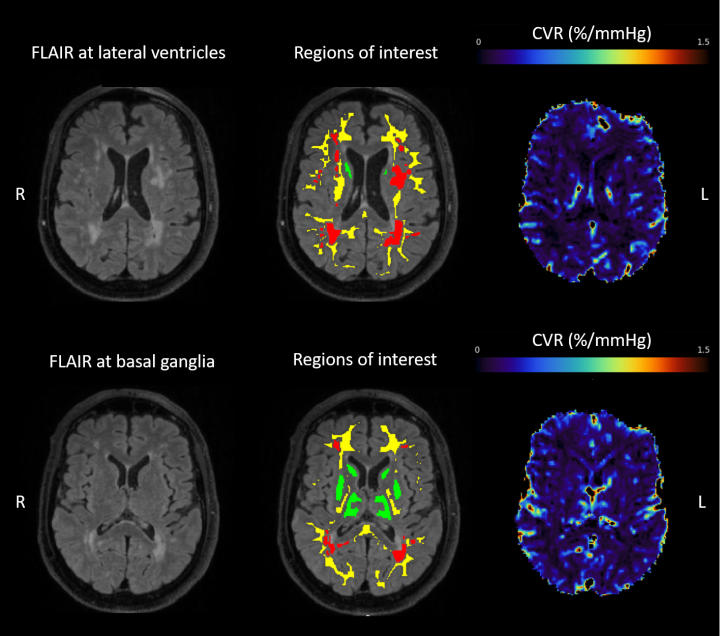
Between February 2018, and April 2022, 75 participants across Europe with sporadic small vessel disease and 26 with CADASIL were enrolled in the trial. The participants were randomly assigned to one of three sequences of antihypertensive treatment, including amlodipine, losartan, or atenolol. The primary endpoint was the change in CVR, measured through blood oxygen level-dependent MRI response to hypercapnic challenge in normal-appearing white matter, over three 4-week treatment periods.
The results of the study were insightful. In participants with sporadic small vessel disease, the change in CVR did not significantly differ between the three study drugs, suggesting that all three medications had a comparable impact on microvascular function.
However, the outcome was different for patients with CADASIL, a hereditary form of small vessel disease. In this group, we detected notable differences in the effects of the three medications on CVR. Amlodipine and losartan both demonstrated improvements in CVR when compared to atenolol.
“This study proves that imaging cerebrovascular reactivity is robust enough not only to be used in multicentre studies, but also that it is sensitive and reliable enough to use as an intermediary outcome in randomised clinical trials. It could be used for testing new drugs in the future.” - Professor Joanna Wardlaw, Chair of Applied Neuroimaging; Head of Neuroimaging Sciences and Edinburgh Imaging; Row Fogo Centre Director.
Notably, the study demonstrated low attrition rates, with 90% of participants successfully completing the rigorous protocol during the COVID-19 pandemic, which involved numerous MRIs, including CVR measurements, telemetric blood pressure monitoring, and multiple drug changes. The TREAT-SVDs trial also underscores the significance of incorporating patients with rare hereditary subtypes of common diseases (such as CADASIL) into clinical studies.
“Microvascular dysfunction plays a crucial role in SVD. This trial allowed us to use CVR, a powerful imaging tool, to investigate how medications commonly prescribed to this patient population for vascular risk-factor management might be impacting microvascular function in unexpected ways. We are immensely grateful to the patients and their families whose invaluable contribution made this research possible.” - Daniela Jaime Garcia, PhD student in translational neuroscience and research assistant in clinical studies of small vessel disease.
The findings of this research raise questions about whether antihypertensive drug classes may differentially impact clinical outcomes in people with small vessel diseases. Further research is needed to better understand how these medications affect the long-term health of individuals with small vessel disease.
You can read the full paper, published in the Lancet Neurology, here.


