BLOG: An MPH student's SLICC project on vaccine hesitancy and proposed communication strategies for Hong Kong
Pandemic preparedness plan for communication strategies to improve vaccine uptake for future novel infectious disease in Hong Kong
By Ka Cheong Chung | MPH Student
On 5 May 2023, the World Health Organization (“WHO”) declared an end to COVID-19 as a public health emergency and suggested “it was a time for deep reflection” and learning from mistakes (WHO, 2023a). WHO also took an initiative to call to action to prepare for future pandemics and emerging global threats (WHO, 2023b).
Vaccination is promoted to be a useful tool to reduce healthcare and economic burden of COVID-19 (WHO, 2022). However, in Hong Kong, despite Government’s efforts to encourage the public to receive vaccination, the uptake rate was only rising slowly, particularly at the start of the vaccination programme (The Standard, 2021). It is also a time for Hong Kong to learn from COVID-19 and think for the future.
Current preparedness and response plan in Hong Kong
In Hong Kong, the current preparedness and response plan for novel infectious disease made by the Food and Health Bureau in 2020 defined different response levels and set out a framework of response with clearly defined structures and efforts among different government departments (Food and Health Bureau, 2020).
Among other things, the current preparedness and response plan included consideration for vaccination in all response levels, but only concerns about liaison with WHO and relevant experts on the latest vaccine development and recommendations (Food and Health Bureau, 2020). There were no plan available for promotion of vaccine uptake in Hong Kong.
My SLICC project on vaccine hesitancy and proposed communication strategies for Hong Kong
Vaccine hesitancy rates in Hong Kong were high – ranging from 21.7% to 31.5% (Lau et al., 2022; Tsang, 2022; Yu et al., 2022). Understanding factors undermining vaccine acceptance would help derive strategies to improve vaccine uptake. As COVID-19 vaccines are new, concern about their safety is one of the discouraging factors for vaccination; and hence, effective communication strategies to disseminate vaccine safety information are essential to promote vaccine uptake.
I have done a Student Led Individually Created Course (SLICC) project to explore determinants for vaccine hesitancy in Hong Kong and communication strategies to improve vaccine uptake. Literature review, talks with people familiar with different stakeholders and sharing with persons working in a public safety monitoring programme of COVID-19 vaccine were done. In this blog, I would like to share my findings of my project and propose a preparedness plan on communication strategies for Hong Kong.
Determinants for vaccine hesitancy
Literature review was performed to identify those determinants in Hong Kong. Determinants could be grouped using the ecological model stratifying them into individual, relationship, community and societal levels and presented in Figure 1.
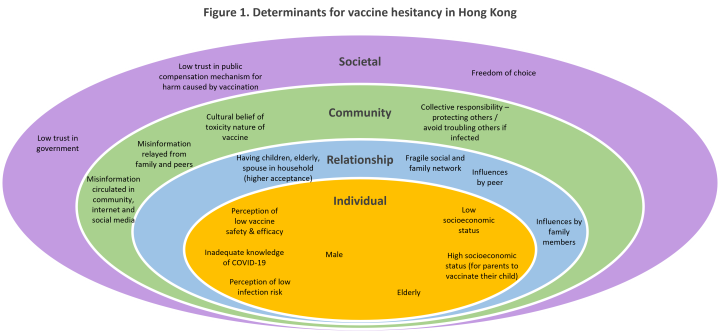
Besides literature review, other relevant factors were also identified from talks with people familiar with different stakeholders.
-
“Wait and see” approach
In general, people knew they or persons under their care need to be vaccinated to prevent complications from COVID-19 infection. However, they would like to see if there were any adverse events happened to other persons similar to them.
The approach was taken up by various stakeholders, such as patients with chronic diseases, elderly, parents of children and persons hesitant for vaccination. Before receiving vaccination, they took other means to protect from infection, including maintaining good personal hygiene, reducing social interactions and wearing face masks. Despite inconvenience, they thought the means were as effective as or even more effective than receiving vaccination. They also waited to see if there would be any incentives for infection, such as extra vacation leave after vaccination.
-
Elderly in care home – elevated risk and difficult for caretakers to make decision on vaccination
Living environment in care home was crowded and there was lack of isolation facilities in care home. Means other than vaccination was not effective neither. It is difficult for elderly to maintain self-hygiene and face masks wearing.
For incapacitated persons, caretakers or attorney understood their elevated risk for infection and complications meaning no other choices than vaccination but found it difficult to make decision on vaccination considering the potential adverse events of vaccination. On the contrary, it is easier for the caretakers or attorney to make “no objection” decision for vaccination (i.e. opt-out approach).
-
Persons refused vaccination – Concerns about lack of evidence to prove safety; also own health more important than convenience and incentives
Persons refused vaccination showed concerns about lack of evidence to prove safety. They thought other means of protection, e.g. wearing mask, reduced social contact, personal hygiene, etc., were effective. They also considered that own health was more important than convenience and incentives from “vaccine pass.”
How might communication tackle vaccine hesitancy in Hong Kong?
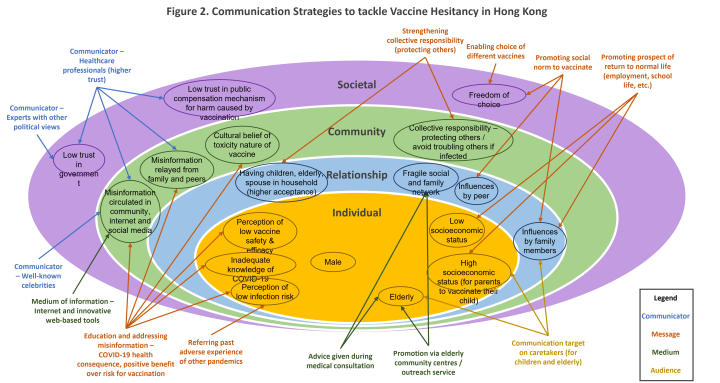
Lasswell’s model consisting of five elements (communicator, message, medium, audience and effect) could be used to guide the discussion of proposed communication strategies (Malikhao, 2020). Figure 2 summarised the communications strategies to tackle vaccine hesitancy in Hong Kong.
Proposed pandemic preparedness plan on communication strategies for Hong Kong
During the sharing with persons working in the public safety monitoring programme of COVID-19 vaccine, it was suggested to learn from COVID-19 pandemic and “do something now” to prepare for future pandemic of novel infectious disease in Hong Kong.
While the public’s memory of the COVID-19 experience remains fresh, it is time to implant and reinforce Hong Kong people’s knowledge on the need for vaccination. Five action areas were identified in the Ottawa Charter for health promotion (WHO, 1986) and could be used as a guide for development of communication strategies to promote vaccine uptake.
-
Building health public policies
Public policy should be in place to support promotion of vaccination in Hong Kong. Current pandemic preparedness plan did not include plan for promotion of vaccination during different response levels. Not only during the pandemic, the public policy for promotion of vaccination should also be implemented in non-pandemic period to prepare for future pandemic.
The policy should also include partnership with the community to pool resources together for communication of messages.
-
Creating supportive environment
There should be approaches to create supportive environment to promote vaccination uptake and tackle various determinants for vaccine hesitancy. Approaches were suggested in the previous section. Approaches could also be innovative, for example, organizing themed concerts, sports events, etc., as well as launching a series of events to attract media coverage and to “let message appear everywhere.”
-
Developing community action
People are better placed to understand concerns of others living in the same community. Volunteers from the community could be recruited to be ambassadors to promote vaccine uptake and identify those members within the same community who are in need for advice and assistance. A community-based support framework should be encouraged and members should also be empowered with resources, knowledge and skills to deliver the service.
-
Developing personal skills
Members of the public should be provided with information to improve public health literacy and understand the need for vaccination. The information could be delivered through workshop, media and social marketing and formal school curriculum. The message for collective responsibility for herd immunities should also be enforced.
People’s immunity to misinformation should be improved through early information dissemination and quick response to misinformation and fake news.
-
Reorientation of health services
Healthcare professionals should be provided with training to strengthen their capacity in communicating with patients, promoting vaccination and responding to vaccine hesitancy (WHO, 2021). Reorientation of health service to a vaccination service integrated with health advice and medical consultation should be explored. Vaccination centre should be redesigned to facilitate delivery of message and people choice.
The reorientation of services should also be supported by government public policy.
Conclusion
COVID-19 pandemic brought huge healthcare burden and economic loss to countries all over the world (WHO, 2022) and it is time to think for our future. Pandemic preparedness plan could guide a quick response in future pandemic of novel infections. Though the plan emphasizes the framework and defined responses at various levels, it could also be more innovative to include promotion of public awareness to prepare for future pandemic. Determinants for vaccine hesitancy and corresponding communication strategies could be cultural and regional specific. Nevertheless, this blog could provide insights and templates for developing a pandemic preparedness plan on communication strategies relevant to different context.
References
Food and Health Bureau (2020). Preparedness and Response Plan for Novel Infectious Disease of Public Health Significance (2020). Available at: https://www.chp.gov.hk/files/pdf/govt_preparedness_and_response_plan_for_novel_infectious_disease_of_public_health_significance_eng.pdf (Accessed: 22 June 2023).
Malikhao, P. (2020). Health Communication: Approaches, strategies, and ways to sustainability on health or health for all. Handbook of Communication for Development and Social Change, 1015-1037.
The Standard (2021). HK will remain an 'isolated island' if elderly refuse jabs: Bernard Chan. Available at: https://www.thestandard.com.hk/breaking-news/section/4/183633/HK-will-remain-an-'isolated-island'-if-elderly-refuse-jabs:-Bernard-Chan (Accessed: 1 March 2023).
World Health Organization (WHO) (1986). Ottawa charter for health promotion, 1986 (No. WHO/EURO: 1986-4044-43803-61677). World Health Organization. Regional Office for Europe.
World Health Organization (WHO) (2021). Communicating with patients about COVID-19 vaccination: evidence-based guidance for effective conversations to promote COVID-19 vaccine uptake. Available at: https://apps.who.int/iris/bitstream/handle/10665/340751/WHO-EURO-2021-2281-42036-57837-eng.pdf (Accessed: 22 June 2023).
World Health Organization (WHO) (2022). Global COVID-19 Vaccination Strategy in a Changing World: July 2022 update. Available at : https://www.who.int/docs/default-source/coronaviruse/global-covid-19-vaccination-strategy-in-a-changing-world---july-2022-update.pdf (Accessed: 1 March 2023).
World Health Organization (WHO) (2023a). WHO chief declares end to COVID-19 as a global health emergency. Available at: https://news.un.org/en/story/2023/05/1136367 (Accessed: 22 June 2023).
World Health Organization (WHO) (2023b). WHO launches new initiative to improve pandemic preparedness. Available at: https://www.who.int/news/item/26-04-2023-who-launches-new-initiative-to-improve-pandemic-preparedness (Accessed: 22 June 2023).

