Accelerated waning of COVID-19 vaccine immunity in obesity
May 2023: New research, published in Nature Medicine, shows that obesity accelerates the loss of COVID-19 vaccination immunity
Accelerated waning of the humoral response to SARS-CoV-2 vaccines in obesity
van der Klaauw, A.A; Horner, E.C; Pereyra-Gerber, P; Agrawal, U; et. al.
Nature Medicine
Published online on: 11 May 2023
Available online at: https://doi.org/10.1038/s41591-023-02343-2
Download the infographic (PDF)
This infographic was created by EAVE II Communications & Engagement Officer, Gabriella Linning
Summary in plain English
Obesity is defined as a Body Mass Index (BMI) of more than 30kg/m2. In England, around 25% of the adult population are obese. Severe obesity or a BMI of more than 40kg/m2, affects 3% of the UK population. People under 18.5kg/m2 are clinically underweight.
Find out more about Body Mass Index [National Health Service]
Obesity has already been shown to be a major risk factor for developing severe COVID-19. Obesity is also linked with other diseases that increase COVID-19 risk. This includes:
- Type 2 diabetes
- High blood pressure (hypertension)
- Long-term kidney disease (chronic kidney disease, CKD)
- Heart failure.
Why did we carry out this research?
Vaccines have already been shown to lower the risk of COVID-19 hospital admissions and deaths (‘severe/serious illness’).
However, the effect of weight on immune responses to current COVID-19 vaccines is unknown. Previous research has shown that for influenza, rabies and hepatitis vaccines, having obesity can reduce a person’s immune response.
We wanted to understand the relationship between weight and immune protection from vaccines. This information will help to inform policy for people who are over or under the recommended BMI.
What data did we use?
To understand this relationship, we looked at two main types of data:
- Population-level data from health records
- Laboratory (lab) test results from individuals.
We used the EAVE II dataset to look at serious COVID-19 for the Scottish population.
Find out more about EAVE II (Early Pandemic Evaluation and Enhanced Surveillance of COVID-19)
Our lab test results are from the SCORPIO study. They include immune response data for 26 people with severe obesity and 40 people with a normal weight. The tests give data on antibodies and immune cell behaviours.
Find out more about the SCORPIO study [University of Cambridge]
Find out about antibodies and immune cells [British Society for Immunology]
What did we find?
In this dataset, there were 1.7 million people who had 2-3 vaccines and a BMI record. Of these, 0.5 million had obesity and more than 98,000 had severe obesity.
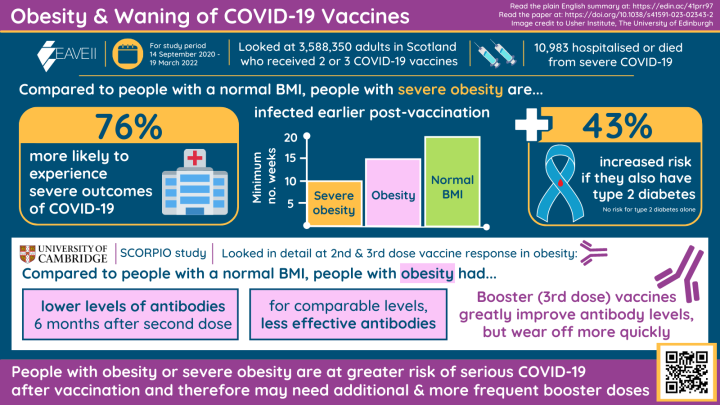
Between 14 September 2020 and 19 March 2022, there were 10,983 people who were admitted to hospital or died due to COVID-19 after 2-3 vaccine doses.
Risk of serious COVID-19 illness after vaccination
Our analysis shows that people with severe obesity were 76% more likely to be admitted to hospital or die with COVID-19. This is compared to people with a normal BMI (18.5 to 30kg/m2). To a lesser extent, people who had obesity or were underweight were also at higher risk of serious COVID-19 illness or death.
We found that people with obesity became seriously ill sooner after their second vaccination. The typical timeframe was:
- 10+ weeks for people with severe obesity
- 15+ weeks for people with obesity
- 20+ weeks for people of normal weight.
Further analysis confirmed that higher BMI is linked to quicker loss of immune protection.
Obesity and linked conditions
We found that people with severe obesity with Type 2 diabetes were 43% more likely to be seriously ill than those with severe obesity alone. Type 2 diabetes alone was also a small risk factor.
There was no further increased risk from having heart disease, heart failure, asthma or chronic kidney disease as well as having (severe) obesity.
Immune responses after a second vaccine
Lab tests can help us understand the underlying reasons for different immune responses.
We found that the quality, but not quantity, of antibodies was reduced in people who had severe obesity, compared to people of normal weight. Antibodies produced by people with severely obesity were less effective at neutralising the SARS-CoV-2 virus, because they were not able to bind to the virus with the same strength.
In people with severe obesity, a smaller variety immune cells were able to recognise important parts of the virus. However, some ‘T cell’ responses were similar for both groups. These T cells control the activity of other immune cells, including making antibodies.
Effects of a booster vaccine
The antibody levels of both groups increased greatly 28 days after their third dose or booster vaccine. However, the protective effect of the booster wore off quicker for people with severe obesity.
Why is this research important?
In this research, we have shown that vaccinated people outside the healthy BMI bracket stay at higher risk of serious COVID-19 illness. The protection offered by vaccines does not last as long for people with obesity.
This appears to be because the immune systems of people with obesity react differently to vaccines.
This research is important because it suggests that more frequent booster vaccines may be needed to offer people with severe obesity continued protection against COVID-19. Further research may be needed to determine the best timing for further vaccines.
Note
This plain English summary was written by EAVE II and Long COVID project's Patient and Public Involvement (PPI) Lead Dr Lana Woolford in consultation with members of the Long COVID PPI panel and data analysts.


