Neurological complications after first dose of COVID-19 vaccination and SARS-CoV-2 infection
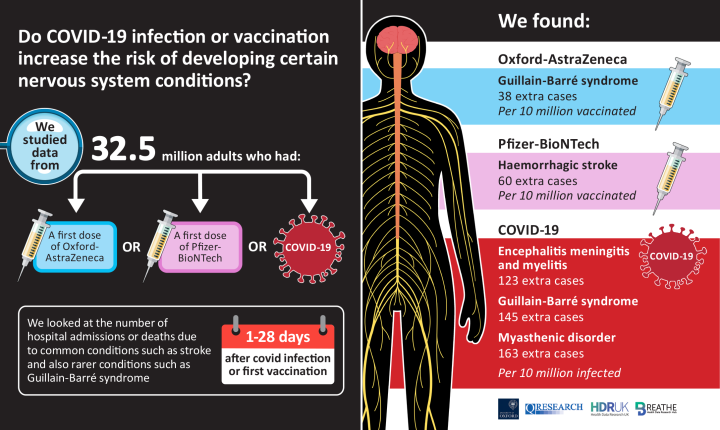
October 2021: Vaccine data analysis from England and Scotland, published in the Nature Medicine, looks at possible links between conditions of the nervous system and COVID-19 infection and vaccination.
Neurological complications after first dose of COVID-19 vaccination and SARS-CoV-2 infection
Patone, M., Handunnetthi, L., Saatci, D et al.
Nature Medicine
Published online: 25 October 2021
Available via Nature Medicine (online): https://doi.org/10.1038/s41591-021-01556-7
Download the infographic (PDF)
This infographic was created by the Usher Institute's Graphic Designer, Dawn Cattanach
Summary in Plain English
The Oxford-AstraZeneca (ChAdOx1) and Pfizer-BioNTech (BNT162b2) vaccines were shown to be safe and effective in clinical trials, and were introduced to the UK and globally from 8 December 2020 onwards.
As people have been vaccinated – in the tens of millions – more data have become available. Individual case reports and small studies in certain populations have identified a possible link between coronavirus (SARS-CoV-2) infection or vaccination and very rare conditions of the nervous system. The nervous system sends and receives messages from the brain, spinal cord and nerves.
Why did we carry out this study?
Studying national data that are routinely collected about people’s health can help us to identify rare disease and potential risks after COVID-19 infection or vaccination that don’t show up in smaller clinical trials. This in turn will help doctors to recognise any rare complications.
We wanted to look at the risks of being admitted to hospital or dying of nervous system conditions to see whether they might be associated with either COVID-19 infection or vaccination.
What data did we use?
To do this, we looked at linked data on hospital admissions, COVID-19 vaccination, COVID-19 infection and death records for 32.5 million people aged 16 or older in England. We looked at people’s risk of nervous system conditions in each of the four weeks after either the first dose of a vaccine or a positive COVID-19 (PCR) test, as well as over the 1-28 days period.
In our analysis, we compared each person’s risk before and after either infection or vaccination. This helps to account for the way in which each person’s health and their personal circumstances (e.g. sex, age, ethnic origin) is different.
We checked the vaccine risk results using routinely collected data from just under 3.1 million vaccinated people in Scotland. This information is held in the EAVE II platform.
What nervous system conditions did we investigate?
We looked at seven different conditions of the nervous system. These are conditions that have been reported in patients following COVID-19 infection or vaccination and may require people to be admitted to hospital. Some, like stroke, are fairly common in the general population. Others, like Guillain-Barré syndrome, are rare.
- Acute central nervous system (CNS) demyelination – when the protective layer (myelin) around nerves becomes damaged in the brain and spinal cord, over a short period of time.
- Encephalitis, myelitis and meningitis – inflammation/swelling of the brain (encephalitis), spinal cord (myelitis), and the membrane which covers the brain and spinal cord (meningitis).
- Guillain-Barré syndrome – damage to the nervous system, which causes numbness and weakness. This happens mostly in the arms and legs. In severe cases, it can affect people’s breathing.
- Bell’s Palsy – a short-term weakness in, or being unable to move, one side of the face.
- Myasthenic disorders – a group of conditions resulting in muscle weakness. These can affect most parts of the body but commonly affect muscles that control the eyes, face and throat.
- Haemorrhagic stroke – a stroke caused by bleeding in the brain.
- Subarachnoid haemorrhage – bleeding in the space between the brain and surrounding membranes.
What were the results?
Of the 32.5 million vaccinated people in England included in the study, just over 2 million had a positive COVID-19 test, either before or after vaccination. Around 1.8 million of these people tested positive before being vaccinated.
COVID-19 infection
In our analysis of data from people in England, we found a significant link between COVID-19 infection and an increased risk of three of the seven conditions listed above over the 28 days after a positive PCR test for COVID-19:
- Guillain-Barré syndrome - extra 145 cases per 10 million people infected
- Encephalitis, myelitis and meningitis - extra 123 cases per 10 million people infected
- Myasthenic disorders - extra 163 cases per 10 million people infected.
The risk of developing Guillain-Barré syndrome in the 28 days after having a COVID-19 infection was over five times higher than the usual risk.
COVID-19 vaccination
We found that people also had an increased risk of developing Guillain-Barré syndrome within 28 days of having the Oxford-AstraZeneca vaccine. Our analysis found an excess of 38 cases of Guillain-Barré syndrome per 10 million doses of Oxford AstraZeneca vaccine, compared to the 145 cases per 10 million people with a COVID-19 infection. This result was confirmed when we repeated the analysis using the data in Scotland.
There was an increased risk of having Bell’s Palsy together with Guillain-Barré syndrome after the Oxford-AstraZeneca vaccine. Clinically, this is likely to represent a variant of Guillain-Barré syndrome with facial weakness, in line with the emerging case reports after the Oxford-AstraZeneca vaccine.
In the analysis of patients based in England, we found a slightly increased risk of having a haemorrhagic stroke after having the Pfizer-BioNTech vaccine. However, when we repeated the analysis in Scotland, this wasn’t the case.
What will we do next?
Overall, the findings from this study show that the risks of nervous system complications linked to COVID-19 infections are far greater than the risks linked to COVID-19 vaccinations; highlighting the benefits of the on-going vaccination programmes. This analysis provides important information about which diseases of the nervous system are likely to be linked with COVID-19 infection or vaccination.
This information will help doctors to recognise these rare complications in their clinical practice and provide appropriate care for their patients. It should also help in planning for the healthcare needs of patients living with long-term nervous system disease as a result of COVID-19.
We will continue to monitor the potential risks of COVID-19 infection and vaccination in England and Scotland, as social distancing and other restrictions ease and younger people are vaccinated.
This research was led by Professor Julia Hippersley-Cox at The University of Oxford, as part of QResearch, with validation in Scotland provided by EAVE II.
Related information
QResearch website - University of Oxford
Note
This plain English summary and infographic were created with the support and feedback of the EAVE II Public Advisory Group (PAG). This summary in particular was reviewed by Lynn L.
To learn more about the PAG, see: Our EAVE II Public Advisory Group (PAG) | The University of Edinburgh


