SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland
January 2022: Research published in Nature Medicine looks at COVID-19 disease and vaccination in pregnant women in Scotland, and the impact this has had on their health.
SARS-CoV-2 infection and COVID-19 vaccination rates in pregnant women in Scotland
Stock, S.J.; Carruthers, J.; Calvert, C.; Denny, C.; et. al.
Nature Medicine
Published Online: January 13, 2022
Available online at: https://doi.org/10.1038/s41591-021-01666-2
This infographic was created by the Usher Institute's Graphic Designer, Dawn Cattanach
Summary in Plain English
Having an infection like coronavirus (SARS-CoV-2) can have an impact on the health of a pregnant woman and her baby. The SARS-CoV-2 virus causes COVID-19 disease.
However, pregnant women were not included in initial clinical trials for COVID-19 vaccines before they were first approved for use. Because of this, data were only available from women who were not aware they were pregnant while taking part in a vaccine trial, and from animal studies.
This limited the information that policy-makers, healthcare staff and pregnant women could use to make a decision about vaccines and pregnancy early in the vaccine roll-out.
Guidance for pregnant women having a vaccine has since changed over time and in different countries, based on the availability of evidence. From 16 April 2021, the UK’s Joint Council for Vaccination and Immunisation (JCVI) recommended that pregnant women should be vaccinated, at the same time as non-pregnant women of the same age and health risk.
On 16 December 2021, the JCVI identified pregnant women as a priority group for vaccination.
Current guidance on COVID-19 vaccines for pregnant women [NHS website]
Why did we carry out this research?
Existing research shows that pregnant women are more likely to have severe COVID-19 than non-pregnant women. COVID-19 has also been linked to pregnancy complications, including premature birth and stillbirth.
We wanted to know how many pregnant women in Scotland have had COVID-19 or been vaccinated. We also wanted to understand how having COVID-19, and getting vaccinated, changes the risk of a mother or baby becoming very ill during pregnancy.
This research helps to create evidence-based guidance for pregnant women and the people who support them.
To carry out this research, we used data held in the COVID-19 in Pregnancy in Scotland (COPS) dataset. This contains information from the health records of all women in Scotland who were pregnant on or after 1 March 2020.
We linked this to infection and vaccination status, held in the “Early Pandemic Evaluation and Enhanced Surveillance of COVID-19” (EAVE II) data platform.
Find out more about COPS and EAVE II
We compared the results to the same information for all women aged 18-44 in Scotland. This information is held by Public Health Scotland.
We included people who had at least one vaccination or infection between conception and the end of their pregnancy. We only included infections confirmed using a PCR test.
National Human Genome Research Institute: information on COVID-19 PCR tests
We restricted our analysis of COVID-19 in pregnant women to December 2020 onwards, as testing became a recommendation for anyone receiving maternity care from this point.
What did we find?
Type of vaccine
Up to 31 October 2021, just under 26,000 vaccinations were given to women in Scotland during 18,399 pregnancies. The majority (95%) were first or second doses. Of the vaccines given to pregnant women:
- 79.4% were Pfizer-BioNTech
- 12.4% were Moderna
- 8.2% were Oxford-AstraZeneca.
Most women who had the Oxford-AstraZeneca vaccine were vaccinated early, because they had other conditions that made them clinically vulnerable to COVID-19.
Vaccine uptake
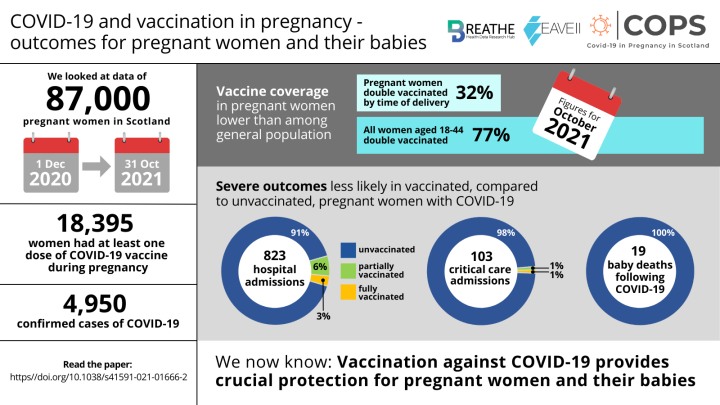
By the end of October 2021, people’s vaccine uptake across Scotland was as follows:
| Vaccine uptake | Pregnant women | All women aged 18-44 |
|---|---|---|
| At least one dose | 43% | 85% |
| Two doses | 32% | 77% |
| Third or booster dose | 1% | 7% |
This shows that vaccine uptake was much lower for pregnant women than women of child-bearing age in the general population. It was lowest in pregnant women who are younger or living in deprived areas of Scotland.
SARS-CoV-2 infection and pregnant women
From 1 December 2020 to 31 October 2021, there were just under 5,000 confirmed infections in pregnant women. There were around 91,000 completed or ongoing pregnancies, in just over 87,000 women, in the same 11-month period. This includes women who did not carry a pregnancy to full term.
Infection rates were similar to the general population, reaching a peak in October 2020, January 2021 and September 2021. They were fairly evenly spread throughout the length of a pregnancy.
Overall, 17% of pregnant women with infections were admitted to hospital with COVID-19. Of the 823 pregnant women admitted to hospital, 104 needed critical care.
Pregnant women were more likely to be admitted to hospital with COVID-19 towards the end of their pregnancy. A third of infected women in their third trimester were admitted to hospital, and nearly 1 in 20 needed critical care. However, pregnant women are generally more likely to need hospital-based care towards the end of their pregnancy.
From December 2020 onwards, over three quarters (77%) of COVID-19 cases during pregnancy were in women who had not yet been vaccinated.
During pregnancy, 9 in 10 infections linked to hospital admission, and almost all (98%) linked to critical care admission, were in unvaccinated women.
To date, there has been one maternal death following COVID-19 during pregnancy in Scotland.
Impact of COVID-19 on babies
There were 2,364 babies born to women who had COVID-19 during their pregnancy. Of these, 11 babies were stillborn.
Of the remaining births, 10.2% were premature. Eight babies died within 28 days of birth, all born to women who had not been vaccinated at the time.
The rate of stillbirths and neonatal deaths was:
- 23 per 1000 for babies delivered within 28 days of their mother becoming infected
- 8 per 1000 for babies delivered following COVID-19 at any point during pregnancy
- 6 per 1000 for babies born to women with no confirmed SARS-CoV-2 infection.
The rate of stillbirths and neonatal deaths was slightly lower for vaccinated women than in women who have never had COVID-19.
Why is this research important?
In this research, we confirmed that vaccination uptake is much lower in pregnant women than in the general population.
We have shown that unvaccinated women and their babies are much more likely to become very unwell with COVID-19 during pregnancy.
We also found that there is no evidence of increased risk of stillbirth or neonatal death following vaccination, compared to women who have never had COVID-19.
Our data support the importance of women being vaccinated during pregnancy.
In the future, we will use the COVID-19 in Pregnancy in Scotland (COPS) dataset to look at the effects of COVID-19 and COVID-19 vaccination on other pregnancy complications. This includes miscarriage and birth defects.
If you have been affected by the themes in this article
Sands is the leading stillbirth and neonatal death charity in the UK. Sands exists to reduce the number of babies dying, and to ensure that anyone affected by the death of a baby receives the best possible care and support for as long as they need it.
Sands offers support in a range of different ways. To find out more:
- Visit sands.org.uk/support-you/how-we-offer-support
- Call the helpline on 0808 164 3332
Further information about the risks of COVID-19 infection for mother and baby, and support for decision making about vaccination can be found on the Royal College of Obstetricians and Gynaecologists (RCOG) and Royal College of Midwives (RCM) websites.
Visit the RCOG website – Advice in pregnancy and women who are breastfeeding
University of Edinburgh Press Release
This paper is from the EAVE II connected project, COVID-19 in Pregnancy in Scotland (COPS)
Find out more about EAVE II's connected projects

