Alternative ways of managing your pain
Advice on alternative ways of managing your endometriosis pain
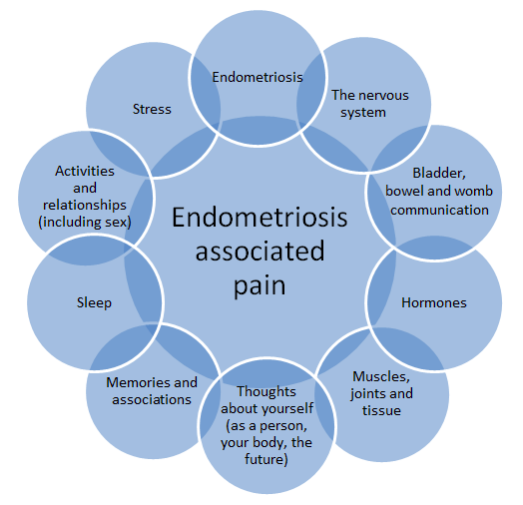
Endometriosis-associated pain is complicated! As you may be aware, there is no relationship between the amount or location of disease and the amount or type of pain experienced. This is also true in other chronic pain conditions such as lower back pain. We know that a variety of different factors can contribute to the experience of pain. Some of the factors known to have a role in chronic pelvic pain are shown in the diagram below. Whilst endometriosis is clearly important, the presence of one or more of the other factors may explain why treatment just targeting the endometriosis (e.g. hormones or surgery) isn’t always successful at removing all the pain.
In addition to changes to your clinical care, it is likely that the COVID-19 pandemic is impacting on many of these other factors, potentially leading to a worsening of your pain currently. We would like to offer you some suggestions as to how you might be able to address these factors during this time. You might be surprised how much help some of these suggestions can be and may even decide that some of them are strategies you wish to continue with even when all of this is over and you can have the treatments previously planned. It is worth remembering that in lots of other conditions associated with chronic pain, a team approach is usually standard care including physiotherapy and psychology, however, in endometriosis we tend to focus only on targeting the disease and only bring in these other options after many years of repeated or unsuccessful treatments.
The nervous system:
The nerves in the spinal cord, the brainstem and the brain itself become more sensitive to painful stimuli over time which is known as central sensitisation. Painful periods over many years may contribute to ‘central sensitisation’. Things that used to only be mildly painful can become very painful. Even non-painful experiences, like clothing or a duvet resting on the skin, can become painful or the nervous system may just generate a painful signal without a trigger at all. People can be more sensitive to a variety of experiences including bright lights and loud noises. You can think of this as like turning up the volume of the pain sensing system. This type of pain is difficult to treat: it doesn’t respond to painkillers traditionally prescribed for endometriosis-associated pain and needs to be approached differently.
If none of the other strategies described here are helping, or your pain feels very like nerve-related pain (burning, tingling, electric-shock like), then it might be worth discussing with your GP whether a trial of a drug targeting nerve pain (known as neuropathic pain) might be a good idea. These drugs are not licensed for endometriosis-associated pain and have never been tested for this reason, however, they are licensed for neuropathic pain and are used in a variety of other chronic pain conditions including fibromyalgia, so your GP will be familiar with them. Possible drugs to consider are:
- Gabapentin
- Pregabalin
- Duloxetine
- Amitriptyline
Your GP will be able to discuss the risks and benefits of these and advise you which would suit you best.
Bladder – Bowel – Womb communication:
Bladder and bowel symptoms are common in women with endometriosis even if they do not have disease on their bladder/bowel. The same nerves supply the womb, bowel, bladder and the top of the vagina and discomfort in one organ may result in discomfort in other areas over time (known as ‘crosstalk’). We also know that bladder and bowel symptoms can be dependent on diet and that bowel symptoms particularly are worsened during times of stress or anxiety.
The current situation is therefore likely to be impacting on bowel and bladder symptoms in at least two ways and therefore potentially increasing the amount of pain from your pelvis. Things you could think about to improve this include:
- Taking care of your diet. The current restrictions on access to shopping and limited availability of supermarket home deliveries means many people’s diets may have changed considerably. A lack of fresh fruit and vegetables or a focus on dried/tinned beans and pulses may well have altered your bowel function causing either diarrhoea or constipation. It might be worth exploring whether there are local farms or shops who are delivering some of your more familiar foods to help with this.
- Avoiding too much comfort food/alcohol. Being stuck inside and a bit anxious/unsettled often means we resort to comfort foods like chocolate and cake or feel the temptation to have a bit more alcohol in the evenings than we would otherwise. These foods can again impact on bowel function and women with sensitive bladders for whatever reason will often describe their pain being worsened by alcohol.
- Staying well hydrated. Not drinking enough fluid as you are out of your routine or don’t feel so thirsty because of a change in your activity levels can lead to constipation and to more concentrated urine which can irritate your bowels and bladder respectively.
- Trying to reduce stress and anxiety. Whilst we understand how difficult this is currently, it is likely to have benefit for your bowel function particularly as well as your pain in general. We offer some suggestions for how to go about this in the section on “Emotional well-being and managing stress” below.
The musculoskeletal system:
Muscles, joints and other tissues can very commonly be involved in chronic endometriosis-associated pain. We often see these become dysfunctional and then begin to create problems of their own. Some examples of this are:
- The pelvic floor muscles become tense and painful which can cause pain during intercourse and/or bladder and bowel issues.
- The back joints can become stiff which can cause pain when sitting or standing.
- The pelvic joints can become irritated causing pain on walking and rolling.
We envisage that lots of people will have increasing levels of musculoskeletal pain as activity levels fall during the pandemic. This is likely to have a significant impact on your general levels of pain if you already experience pelvic pain. Things you could consider to reduce this impact are:
- Making sure you get outside for some daily exercise as long as you stick within current Government recommendations for social distancing/isolation. If long walks flare your pain, then this can just be a slow, gentle walk or bike ride. However, the benefits of being outside for your mental health as well as your physical health are huge.
- Making time within your day to do some gentle “pelvis friendly” exercises at home. You may already have a routine that was given to you by a physiotherapist or personal trainer, in which case please continue with this. Otherwise we have put together a set of exercises that may be helpful to you and are available here:
- Keeping an eye on your diet and your weight. Constipation is likely to worsen any pain from your pelvic floor, whilst carrying excess weight puts a strain on muscles, which if they are already weak can cause or exacerbate pain.
Emotional well-being and managing stress:
Living with chronic pain is incredibly difficult. It is likely to have a big impact on how you think, feel and what you feel/are able to do. The experience of constant/repeated episodes of pain is stressful and can make it difficult to relax. The current situation is likely to have made the situation worse; therefore here are some suggestions for how you can look after your own emotional well-being during this time. As mentioned, you may find that some of them are so helpful that you choose to continue them in the future too.
The importance of taking care of ourselves
It is especially important to consider how we can best take care of ourselves during this unsettling and stressful time. You might be experiencing additional challenges for a number of reasons, including: worries about accessing medical treatment, additional stress and disturbed sleep which may exacerbate pain or reduce confidence to cope, and loss of routine and reduced opportunities for socialising or physical activity, or other things which helped you to cope.
Understandable increased sense of threat
The coronavirus may well contribute to an increased sense of threat. However, for women who have been living with endometriosis, this sense of threat may already be ‘online’ more of the time as it can also be triggered by health concerns, pain, unpredictability and medical treatments. Some common experiences that come along with the sense of threat include:
- Thoughts: I can’t cope, there is nothing I can do, things are out of control, what if….,
- Body: heart racing, palpitations, muscle tension, stomach ache, tearful, poor concentration, pain
- Emotions: Stressed, worried, irritable, numb, disconnected, sad, angry, frustrated, self-criticism
- Behaviour: Push self, withdraw, skip meals/comfort eat, snap at others, stay up late, difficulty relaxing
*** IT IS COMPLETELY UNDERSTANDABLE AND NORMAL TO FEEL LIKE THIS AT THIS TIME ***
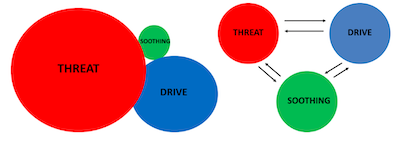
Humans have three basic emotional regulation systems: threat, drive and soothing systems.
All serve very useful functions, but we need balance. The threat system may be especially online at the moment. To maintain balance, enable us to rest and for our well-being we need to bring the ‘soothing system’ online.
Some tips strategies for this are described in the next section.
Tips and strategies for taking care of ourselves:
Establish a routine:
Build in a range of activities into your life so that your time does not feel entirely taken over by worries about your health and the current situation.
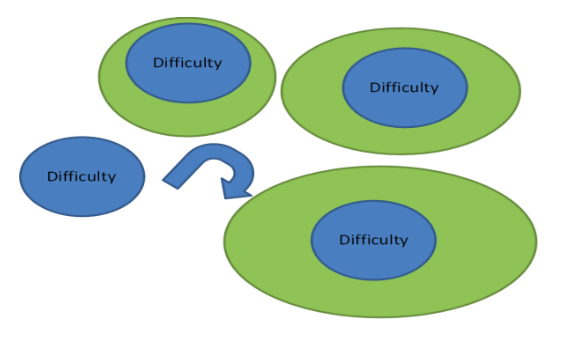
Of course these concerns will be there but see if you can ‘grow’ around the challenges you are facing.
Each day try to tick off a few from this list:
- Being active/exercise
- Contact with others (friends/family)
- Pleasurable activity
- Time to relax
- Do something fun
- Give yourself a challenge (e.g. puzzle)
Limit exposure to ‘threat’ information:
The empty shelves, news, social media, school and shop closures all keep this threat at the fore of our attention. Thoughts and worries about managing endometriosis at this time may add to this and will inevitably affect how we are thinking and feeling. Limit the amount of time you listen to the news, look on social media or spend looking up health information. Try to have some conversations or some allocated time which is ‘threat’ free.
Taking in the good:
Negative events are like Velcro, positives are like Teflon: we notice and remember negative information more easily (e.g. we notice/remember what went wrong in our day, not what went well). In the current circumstances we may need to take some steps to balance our inbuilt negative attention bias by focusing on some of the good in our lives. For example,
- At the end of the day, see if you can think of 10 things you appreciate (e.g. the smile from a stranger, the smell of your coffee)
- Make time for pleasurable experiences and give them your full attention. You can do this for brief experiences (e.g. the feel of the sun on your skin) as well as longer ones (e.g. watch your favourite film)
- Do something kind – call a friend, make a cup of tea for someone, smile at someone
Look after your body:
Try to eat healthily and regularly; if your appetite is low eat little and often, choose things you find easy to eat. Take a bath or long shower. Try to keep active.
Our thoughts:
We may find ourselves overwhelmed with negative thoughts; how we think about a situation will affect how we feel. Remember, thoughts are not facts, and it might be helpful to keep other perspectives in mind, such as….
- I am limited in what I can do, but I will do what I can
- I can’t control many things, but I can look after myself
- This will end, we will get through this
- I’m not alone/others are facing challenges too
This isn’t about positive thinking. It’s about holding a balanced perspective in mind.
Living with uncertainty:
It is common to find uncertainty difficult to live with, but sometimes our need for certainty can end up adding to our problems. For example, we might find ourselves going over and over things in our mind, feeling more stressed or frustrated, but the situation stays the same. Sometimes, no matter how hard we try to solve a problem, there is nothing we can do to change the situation or resolve the issue. Learning to accept situations we can’t change may sometimes be the most helpful thing to do. A helpful question to ask yourself is: Is this a worry I can do something about? If the answer is ‘no’, try the steps for accepting uncertainty (below).
Steps for accepting uncertainty:
- Be aware – What do you notice yourself thinking and feeling when the need for certainty comes up?
- Don’t respond – What can you tell yourself to help you not respond? (e.g. These feelings will pass)
- Let go – What can you do to help you let go of the need for certainty ? (e.g. I can’t fix/change this)
- Focus on the present – See the grounding techniques below.
- Deal with a wandering mind – Notice when your mind wanders, perhaps automatically getting caught up in worry again and again. Each time, gently bring your attention back to the present moment.
Acknowledging and naming emotions:
Acknowledging and naming the emotion, either to ourselves or talking with someone else, can be helpful. Research shows this can help to give perspective and to calm emotions. For example, you could say to yourself “I notice I am feeling overwhelmed; I can see that I am feeling irritable”. Keeping a diary might be helpful.
Grounding techniques:
When overwhelmed with emotion we can feel lost and disconnected from the present moment: our ability to think clearly and rationally may go ‘off-line’. Grounding techniques are a way of helping us to feel a little steadier and manage strong emotions, helping us connect with the present moment – the here and now. They can be quick strategies (like taking five mindful breaths) or longer, more formal exercises (like mindfulness meditation or yoga). Different strategies work for different people, and there is no “wrong” way to ground yourself. The main aim is to keep your mind and body connected and working together. Some ideas include:
- Come into your senses – stop, notice 5 things you can see, close your eyes and notice 5 things you can hear, and then notice 5 points of contact between your body and something else. Breathe. Then open your eyes.
- Take 5 breaths, paying full attention to the sensations of the breath.
- Focus on sensations in your feet as you walk from one place to another.
- Get outside – notice nature around you if you can access this. Feel the air on your skin.
Sleep:
Sleep is incredibly important. We know that poor quality or insufficient sleep makes it difficult to cope with things that you would normally manage fine. There is also increasing evidence that sleep deprivation can amplify pain, such that sensations that were previously only mildly painful become more severe. Even if your sleep is not disrupted by pain it can be difficult to get off to or to stay asleep during these unsettled times. Here are some top tips for getting your sleep back on track during this time:
- Routine: Establish a relaxing bedtime routine and give yourself longer to wind down at bed time (up to 90 minutes can be helpful)
- Keep bed for sleep (if you can): If you spend time in bed for reading, watching TV or resting, your body/mind may not associated bed with sleep. It’s important to create a strong link between bed and sleep by avoiding using bed for other activities.
- Rise time: If you haven’t slept well it can be tempting to have a lie in to catch up. Unfortunately, this is likely to decrease the likelihood of a good night sleep the following night, because you won’t have been awake long enough to build up ‘sleep pressure’ across the day. Set a regular rise time and see if you can stick to it. It might be hard work in the short term but will improve your chances of falling asleep each night. To help with getting out of bed at your rise time, plan some things to help get you going; perhaps a lively piece of music, a nice breakfast or a shower.
- Napping: If you can, it is best to avoid napping as it can lead to a disrupted sleep at night. The longer we are awake, the greater the ‘sleep pressure’ will be at night. If you do need to nap, try to keep it short (20 minutes) and earlier in the day to allow sleep pressure to build up again.
- Avoid stimulants before bed (caffeine, alcohol, nicotine)
- Natural light: Natural light suppresses the production of melatonin (a hormone associated with sleep). Try to avoid bright light before bedtime to promote melatonin production. It is also helpful to expose yourself to lots of natural daylight when it’s time to be awake (particularly early morning). This will help you to feel awake, alert and ready for the day.
- Screens/blue light: Avoid screens for an hour (or more) before bed as the blue light can supress melatonin production.
- Relaxation/mindfulness: Do a relaxation or mindfulness exercise (e.g. look on the internet for progressive muscle relaxation or a body scan) to help your mind and body wind down and ready for sleep.
If you can’t sleep, try not to worry about your sleep and see it as a time for rest – the more you worry, the less you will sleep! Try a relaxation exercise or mundane mental activity (e.g. counting down from 100 in 7’s; remember the details of a walk you know well).
Activities and relationships:
We know that some activities can improve pain whilst others worsen it and this is likely to be different for different women. Similarly some relationships are helpful whilst others can make us feel worse. How we structure our day and interact with other people is likely to have changed significantly since the COVID-19 pandemic and particularly since the stricter government recommendations have come into force. If you have noticed a marked change in your pain (for better or worse...), it might be worth spending some time reflecting on what has changed and how this might be having an impact. If you think these changes have worsened your pain, then you may need to alter the way you structure your day, either to avoid doing things that make the pain worse; give yourself more/longer rest periods; increase or alter your social interactions. On the other hand you may notice benefit, in which case it would be worth remembering these things for the future to see if positive changes could be incorporated into your life going forwards.
Things to consider include:
- Are you doing more activities like housework? If you are normally used to a desk job but are spending your time hoovering or moving furniture around to keep yourself busy, this may have put more of a strain on your muscles or alternatively may have improved the back pain you normally get from sitting all day.
- Are you spending lots of time sitting on the sofa watching TV or listening to music? If you normally keep active, this might be worsening your pain and your mood. On the other hand making some time for relaxation is really important and therefore this bit of “me-time” may actually be making you feel better.
- Are you interacting less with your extended family/friends/work colleagues? This may be making you feel isolated and lonely and thus worsening the situation. In which case why not look into novel ways of linking up. Many people are using technology to have virtual coffee mornings, dinner parties or an evening drink. Alternatively if that technology isn’t available a simple phone call may be enough to help you stay in touch. Or have you noticed that you feel much better not interacting with a certain person? In which case this may be something to think about for the future.
- Is spending 24/7 with your close family stressful or enjoyable? Many people are enjoying the opportunity to play games or watch films with their family that they wouldn’t normally. Maybe this is something you can continue to plan in the future? However, it is challenging to spend all our time at home and this may be even more difficult if you are trying to both homeschool and work from home, or if one of your family is particularly stressed or anxious about the current situation. If you don’t feel safe at home then you should seek some advice, this resource may be helpful: https://www.womensaid.org.uk/covid-19-coronavirus-safety-advice-for-survivors/. If you are in immediate danger, call 999 and ask for the police - the police will continue to respond to emergency calls. If you are in danger and unable to talk on the phone, call 999 and then press 55. This will transfer your call to the relevant police force who will assist you without you having to speak.


