Long COVID prevalence in Scotland similar to stroke and COPD, study finds
Preliminary findings from an EAVE II sub-study were presented to the Scottish Parliament COVID-19 Recovery Committee's inquiry into long COVID.
UPDATE April 2024: Full peer-reviewed paper now published:
Prevalence and risk factors for long COVID among adults in Scotland using electronic health records: a national, retrospective, observational cohort study
Jeffrey, K; Woolford, L; Maini, R; Daines, L; et. al.
eClinicalMedicine, Volume 71
Published online on: 12 April 2024
Available online at: https://doi.org/10.1016/j.eclinm.2024.102590
[Below article unchanged from 24 March 2023]
Read our full summary in plain English for this paper
What we have [with the EAVE II study] is exceptional because it looked at 5.1 million adult Scots. I am not aware of previous linkage of that size and that power and potential. So I think it is extremely exciting to see that such linkage is possible.
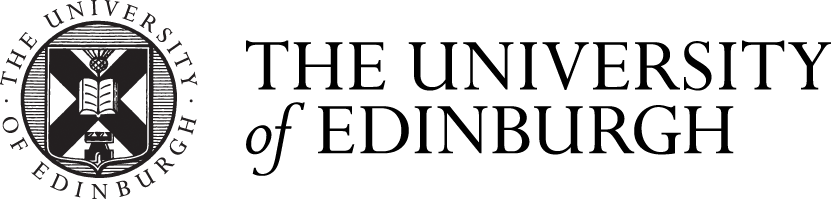
New evidence from the EAVE II Long COVID sub-study suggests that nearly 91,000 adults in Scotland (1.8% of the adult population) experienced long COVID between March 2020 and October 2022.
The study, which has been submitted for peer review, also found that long COVID cases were disproportionately common among people who are: female, middle aged, living with two or more pre-exiting health conditions, overweight or obese, advised to shield or immunosuppressed.
According to Dr Luke Daines, Project Lead and Clinical Research Fellow from the University of Edinburgh, these results are a massive step toward understanding the impacts of long COVID in Scotland,
We found that long COVID is common in Scotland, with a similar prevalence to conditions such as stroke, COPD or atrial fibrillation. Our results provide up-to-date information on the prevalence of long COVID in Scotland, including demographic data on those most affected which has been sought after by the public.
These results were presented this morning to the Scottish Parliament COVID-19 Recovery Committee as part of their ongoing long COVID inquiry. During the session, EAVE II was represented by Professor Chris Robertson from the University of Strathclyde.
- Video: EAVE II at Scottish Parliament Long COVID Inquiry (full)
- A video summary of EAVE II's contributions and mentions during the 9 March 2023 long COVID inquiry evidence session.
Clinical codes rarely seen in primary care records
The study looked at the electronic health records of over 5.1 million adults living in Scotland and used four different methods to identify long COVID cases.
-
Clinical codes – long COVID specific codes entered into a patient's records by their General Practitioner (GP)
-
Free text in primary care records – Notes or non-coded information recorded into a patient’s health records by their GP (e.g. about the symptoms they are experiencing)
-
Sick notes
-
Novel operational definition – An analytical definition of long COVID developed by the study team based on patients having a positive COVID-19 test and two or more features (i. e symptoms, clinical investigations or prescriptions) in their records that suggest long COVID
Most cases were identified by the novel definition, whilst clinical codes identified the least number of cases.
These findings support previous results from England, which also suggested long COVID clinical codes are underutilised by GPs.
According to Dr Karen Jeffrey, the study’s Lead Data Analyst from the University of Edinburgh, there are several reasons for this,
Clinicians primarily record data in Electronic Health Records for non-research purposes and coding multiple symptoms may be prohibitively time-consuming. Long COVID codes may be particularly under-utilised due to lag between cases emerging and codes being made available, clinicians’ lack of familiarity with the codes or reluctance to commit to the diagnosis of long COVID due to clinical uncertainty.
Groups at risk
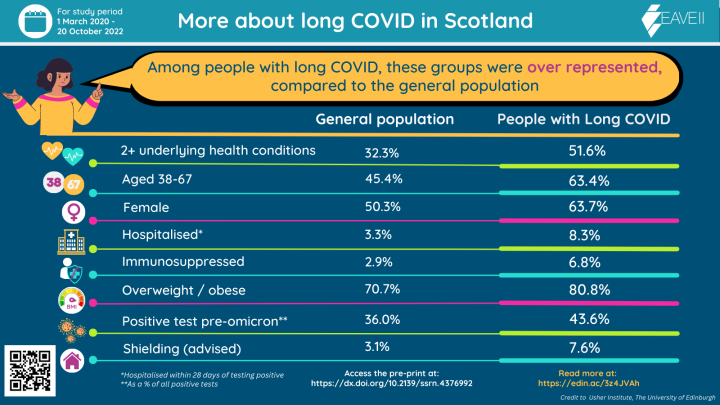
The study also identified several groups who were disproportionately affected by long COVID compared to Scotland’s general population. These included:
-
Female;
-
Aged 38-67;
-
Overweight or obese;
-
Living with two or more underlying health conditions;
-
Immunosuppressed;
-
Advised to shield;
-
Hospitalised within 28 days of testing positive for COVID-19; and
-
Tested positive for COVID-19 before the Omicron variant became dominant in the UK.
A “substantial underestimate”
However, these findings are likely a substantial underestimate of how many people in Scotland have been, or continue to be, impacted by long COVID.
Earlier estimates from self-reported surveys, such as the Office for National Statistics, are much higher, ranging anywhere between 2-5%.
As Dr Jeffrey explains this is because the analysis depends on how long COVID patients and GPs engage with each other,
We looked at patients' health records to find out how many people in Scotland have long COVID, but it's possible that some cases were not identified. If a person with long COVID did not talk about their symptoms with a doctor, or if the doctor did not record all the information needed to identify long COVID, those cases would not be included in our findings.
Dr Daines also adds,
The methods we used depend on someone with long COVID attending health services, but we know that not everyone with long COVID will present. This can be for multiple reasons including putting up with symptoms, not feeling there is any point due to lack of treatment options, fears of not being taken seriously, difficulty in accessing health care and so on. These interactions with primary care would also need to be identifiable, either through coding, free text or the operational definition.
The paper also outlines how selection biases and reporting inaccuracies may impact the results of self-reported surveys.
Future directions
EAVE II’s long COVID sub-study is now working towards creating a model which will help predict which groups of people are more likely to develop long COVID.
The researchers have also recommended that free text analysis of electronic health records be used in any future long COVID surveillance work.
Relevant links
Read this paper's full summary in plain English
Read the pre-print in The Lancet
Read the supplementary materials
Find out more about EAVE II’s long COVID work
Find out more about why long COVID clinical codes are underutilised by GPs
-
Meeting minutes from the 23 February 2023 long COVID inquiry session