BLOG SERIES – Asthma outcomes: Primary care perspective | Dr Katherine Hickman
Dr Katherine Hickman, GP, Vice-Chair of the Primary Care Respiratory Society, and Primary Care Lead for the National Asthma and COPD programme talks us through how she believes change in asthma care in primary care can be driven by small behavioural changes
For many years, respiratory care hasn’t been prioritized, either locally or nationally.
I believe not all but many of us have developed bad habits:
- We’re not making accurate diagnoses of asthma patients
- We’re not discussing what’s going on in patients’ airways, so they leave the room without a clear understanding of bronchial constriction and inflammation
- We’re not tackling smoking properly
- We’re not making sure that patients know which inhalers to take and when
- We’re not discussing adherence or co-creating personal asthma action plans (PAAP) so that patients know how to manage their asthma at home and also what to do in an emergency
Bad habits have become ingrained.
We can recognize that we know what we should be doing, but we don’t always know how to change.
Behaviour change is key
Your weakest link determines what makes a behavior hard to do
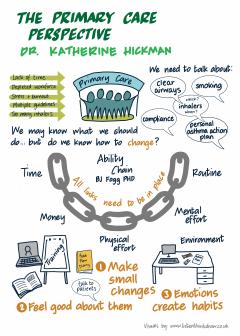
BJ Fogg is a behaviour change scientist at Stanford University and he talks about the Ability Chain.
If we think about it, asthma care can be broken down into components; individual clinician behaviours. For each behaviour, we need to ask ourselves:
- ‘Do I have enough time to do it?’
- ‘Do I have enough money?’
- ‘Am I physically capable?’
- ‘Do I have the mental energy?’ and,
- ‘Does this behavior fit into my current routine, or does it require me to make adjustments?’
It’s not as simple as giving nurses more time to do a review, because if they haven’t been trained to fill out a PAAP, it won’t happen. Equally, a GP can have the physical capability to demonstrate inhaler technique and as many placebos as possible on their desk, but if they only have a ten-minute consultation, and they’ve already covered two problems, it’s unlikely to happen.
Implementing change in practice
For each behavioural component of asthma care, we need to ask ourselves, ‘What is making the behaviour hard to do?’ i.e. which part of my ability chain is broken?, and ‘How can I make the behaviour easier to do?’
There are three approaches we can take:
- Increase your skills. You watch videos, you attend webinars, you go to face-to-face learning (when possible). You learn how to talk to a patient about how to use a peak flow diary, how to create a PAAP, and learn to talk to patients about the pathology of asthma so they have a true understanding of the nature of their asthma. You also understand how to talk to patients on the importance of inhaled corticosteroid adherence and over-reliance of the salbutamol inhalers.
- Tools and resources. How can I change my environment so that I make it easier to do the right thing? I have placebos readily available. I have PAAPs either printed out or embedded in my clinical system. The paper slide rule is on my desk ready to be used with patients, or available on my desktop. Airway models are easily accessible and on my desk so I can talk about them with patients. I have quick access to inhaler videos to be able to text the link to patients there and then.
- Make small changes. If all this is too overwhelming then it is OK to start small, in fact tiny and consider using BJ Fogg’s Tiny Habits® method, and remember to celebrate all successes. Emotions create habits.
After I prescribe an inhaler, I will get out a placebo inhaler and celebrate. After I prescribe a salbutamol inhaler, I will automatically check the inhaled corticosteroid adherence and celebrate. After a patient walks in for their asthma review, I will open up their PAAP and celebrate.
As part of an initiative to reduce our carbon footprint in West Yorkshire & Harrogate we are focusing not on switching patients to dry powder inhalers (DPIs) but focusing on good asthma care. Five clinicians are being trained in the Tiny Habits method and will be teaching patients on how to remember to take their preventer inhalers with the hope being that good adherence will lead to good asthma control and a natural reduction in salbutamol metred-dose inhaler (MDI) use and ultimately a reduction in our overall carbon footprint. These same clinicians will also be working with their colleagues to support them in changing their behaviours when managing patients with asthma.
The most common way people give up their power is by thinking they don’t have any.
Change starts with you and you as an individual. We all have the power to change. If nothing else, COVID has shown us that we can change and adapt fast. Good asthma care starts with the individual. For every patient we get it right for, we may end up preventing an asthma attack, a visit to hospital or even save a life.
Watch the webinar again
Watch our webinar ‘Why is the UK still struggling to significantly improve asthma outcomes?’ hosted in association with the Primary Care Respiratory Society.
Image credit: www.listenthinkdraw.co.uk

