Blog - What are the problems with ageing and how will the ACRC help?
Our first blog post is from the Director of the Centre, Bruce Guthrie, and outlines the challenge posed by ageing and multimorbidity to health and social care, and the role of the ACRC in finding solutions.
Posted by Prof. Bruce Guthrie on 1st July 2021
If you would like to speak to us about the issues raised in this blog, or have any suggestions of topics you would like us to cover in future posts, please contact us.
What is the problem?
People in the UK and many other countries are living longer. Increasing life expectancy is to be celebrated, but it poses major challenges for many individuals and families, and for both public and private sectors. The problem is not simply that people are living longer, but are living longer in poor health. In the UK, life expectancy has grown faster than healthy life expectancy, with men now expected to spend 16 years of life in poor health, and women 19 years. The challenges posed by ageing populations are broad. Increasing numbers of people are living with multiple health conditions (known as multimorbidity), and experience long-term physical and mental frailty that needs managing. Multimorbidity rapidly increases with age with the majority of over-75s having at least three major chronic conditions. Multimorbidity is strongly associated with worse physical and mental function and reduced quality of life, which drives the need for support from family or health and social care services in later life.
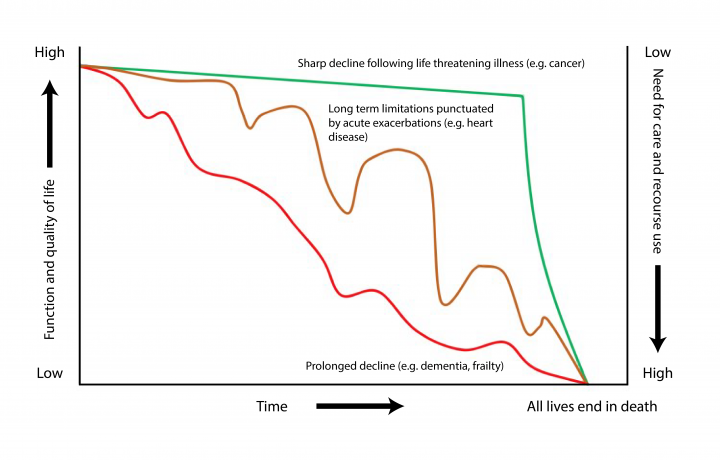
Looking back from death, it is often straightforward to see when someone’s physical and mental function and care needs changed. However, our ability to predict future needs is poor, and our care systems are not optimally set up to minimise future ill-health or mitigate the effect of functional decline on quality of life and independence.
Trajectories of function and quality of life in the last few years of life (adapted from https://www.bmj.com/content/330/7498/1007).
Why does this matter?
Many people in later life are taking large numbers of medicines and attending several appointments for separate conditions rather than effectively managing the complexity of their individual circumstances. Social care, such as help in the home, is more focused on function and generic needs, but is typically low tech with limited integration with healthcare, and both health and social care fail to make best use of their data and human resources. Neither health nor social care are well orientated to support family, friends and neighbours who are critical caregivers. Both tend to treat people in later life as relatively passive ‘recipients’ of care, but we are all both cared for and caregivers at different points in our life, and people with declining health usually remain active participants in society including as caregivers in their own right. The challenges posed by an ageing population are broad, and can only be addressed by people from many different areas of society working together.
What is the solution?
Our aim is to transform care for people in later life using personalised care enabled by data science, artificial intelligence (AI) and assistive technologies and robotics. We want to embed this in systems of health and social care which are highly responsive to the wishes, priorities and needs of individual people in later life.
How will the ACRC help?
We have chosen to focus on care in later life which is an immediately pressing priority that is already threatening the viability of health and social care systems and yet is ripe for data-rich solutions. All interventions in this context will be complex because they require integrating several interdependent elements in a changing organisational and social context. New technologies alone will not be effective unless they are integrated in professional workflows, in the NHS and private care sector) which themselves need to better identify and address individual context, priorities and needs, requiring detailed work with people in later life and carers over time to really understand what matters most to them.
Each element requires development and evaluation in its own right (prediction tools have to be shown robustly to predict; assistive technologies have to truly assist; new models of care have to appropriately respond to individual circumstances). However, all elements then need to be integrated and implemented at scale to demonstrate benefit and cost-effectiveness. The key value of our approach is that it allows the whole to be greater than the sum of the parts, by ensuring supported cross-disciplinary integration and cross-sectoral collaboration embedded in real-world care delivery from the outset.
Our core principle is that the person in later life must be at the heart of everything we do.
The ACRC will enable data-driven, personalised and affordable care that delivers independence, dignity and a high quality of life for people living in their own homes or in supported care environments. We are working with patients and members of the public across our work.
What are we already doing?
The ACRC has been up and running since the end of 2020, and involves over 30 academics from the Universities of Edinburgh and Newcastle. Over 25 new researchers and other staff have been brought on board, bringing a wealth of experience from a range of disciplines (from medicine, through engineering and informatics, to social sciences and architecture). We also have 13 PhD students joining our Academy for Leadership and Training in Advanced Care in September 2021, to develop the next generation of leaders in this field who will be both excellent in their core disciplines and skilled in working widely across disciplines and sectors. We will be holding a formal launch event later this year, and updates, journal articles, briefing papers, other blog posts about the research and outputs will be on the website in the coming weeks and months.

