New insights into how severe brain cancer evades immune attack
Cancer Research UK Edinburgh Centre researchers uncover mechanisms underlying immune evasion in Glioblastoma multiforme (GBM): April 2021
Glioblastoma multiforme (GBM) (also called glioblastoma) is a fast-growing tumour type that develops from star-shaped glial cells (astrocytes and oligodendrocytes) that support the health of the nerve cells within the brain. Treatment options are limited and just a quarter of glioblastoma patients survive more than one year.
One of the reasons glioblastoma is so hard to treat is because it has many distinct types, in terms of the genetic makeup and how those genes are expressed (transcriptional profile). In one of these distinct tumour subtypes (mesenchymal glioblastoma), the tumour supresses the immune environment around the cancer cells making it harder for the body to defend itself against those invasive cells.
In a recent study, titled “Glioblastomas acquire myeloid-affiliated transcriptional programs via epigenetic immunoediting to elicit immune evasion” and published in the journal “Cell”, investigators from the University of Edinburgh, the University College London and the Brown University identified the way in which glioblastoma can evade the body’s own immune response by using signals normally found in immune cells.
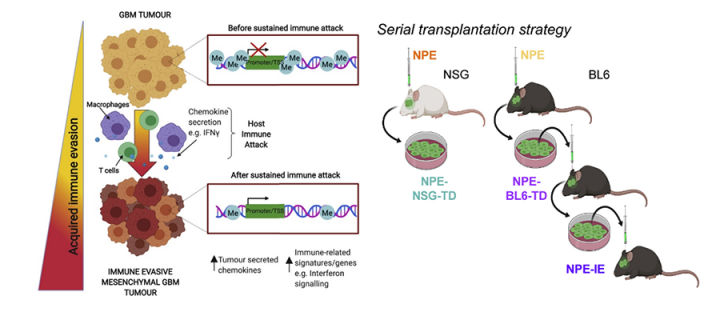
By engineering immune-resistant glioblastomas in mice, the team have shown that the cancer cells mimic the way genes are expressed in immune cells, overcoming the natural immune response to cancerous cells. Researchers engineered glioblastoma mutations into brain (neural) stem cells using the CRISPR/Cas9 gene editing technique. Mice transplanted with these cells developed glioblastoma.
Innovatively, the team subsequently removed some of these glioblastoma cells and transplanted them into the brain of a new mouse. This process was then repeated, taking cells from the new mouse and transplanting them into a third mouse. With each transplantation, the cells altered in response to serial immune attack, resulting in cancer cells that could evade the immune system.
Professor Steven Pollard, who led the study, and his colleagues were surprised to find that the resulting cells were not genetically different, but that there was a profound difference in which genes were switched on or off (the transcriptional profile) in those cells.
Cells produce proteins according to a blueprint laid out in the genes, however which genes are switched on or off is controlled by molecules known as transcription factors. The transplanted cancer cells were found to have adapted by highjacking transcription factors that are normally used by the immune system.
The study found that the mouse glioblastoma is representative of the human disease, as cells from glioblastoma patients showed a similar transcriptional profile to those from the transplanted mice. The work was supported by funding from CRUK and offers a new way to study immunotherapies for glioblastoma.
We uncovered an unexpected arms race between the cancer cells and the immune system. Surprisingly as the tumour cells are attacked by the immune system, they have a plasticity to change the sets of genes which are turned on, and ‘hijack’ molecular processes that enable them to hide from the immune attack. The new experimental tools we’ve built should now have practical value in helping in the development of new treatments for these brain tumours that harnesses the ability of the immune system.
Related Links
- Article in Cell: https://www.sciencedirect.com/science/article/pii/S0092867421003512
- Professor Steven Pollard Group website: https://www.ed.ac.uk/cancer-centre/research/s-pollard-group
- Information about glioblastoma: https://www.thebraintumourcharity.org/brain-tumour-diagnosis-treatment/types-of-brain-tumour-adult/glioblastoma/
- Information about gliomas: https://www.cancerresearchuk.org/about-cancer/brain-tumours/types/glioma-adults

