Enhancing lipid signals helps control severe asthma, study shows
CIR researchers show that activating specific inflammation lipids can reduce the severity of asthma symptoms and other lung allergies.
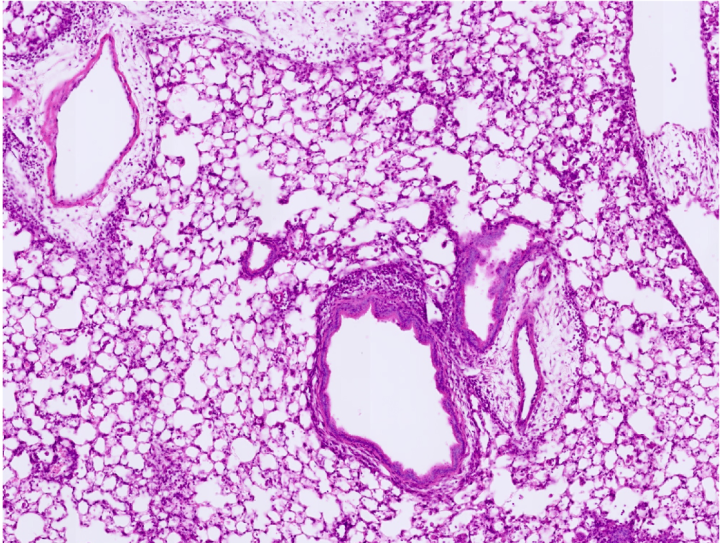
A team of researchers from the Yao Lab at the Centre for Inflammation Research (CIR) have discovered a new potential way to control severe asthma. By studying lung inflammation in mice, they have identified certain proteins and a specific gene that, when activated, can reduce allergic immune responses in the lungs.
Current asthma treatments
Asthma is a chronic, allergic inflammatory lung disease that can affect both children and adults. There are more than 300 million people worldwide living with asthma, and it causes hundreds of thousands of deaths each year. Asthma symptoms and asthma exacerbations can be controlled by various medicines such as steroid hormones and antibiotics. However, the effects of such drugs stop rapidly when they are discontinued. Moreover, no current treatments can completely cure asthma.
Non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin, are one of the most prescribed medicines. NSAIDs have been widely used to treat various inflammatory conditions such as pain, fever and arthritis. But nearly one third of patients with asthma have a reaction to NSAIDs or aspirin, called NSAID-exacerbated respiratory disease (NERD). NERD usually happens in patients with severe asthma, and can be life threatening.
The PTGER2 gene
Although there has been significant research into asthma, many questions still remain, such as how NERD is developed and how it can be treated. It is known that patients with NERD have unbalanced levels of lipids or fats that are associated with inflammation. A feature of this imbalance is under-production of a lipid called prostaglandin E2 or PGE2 in NERD patients. PGE2 in the environment outside the cells can be sensed mainly by two proteins called EP2 and EP4. The EP2 protein if produced by a gene called PTGER2. Interestingly, alterations in the PTGER2 gene, which leads to inactivate EP2, is also associated with NERD. However, it is not clearly known why reduction of PGE2 or inactivation of EP2 happens in NERD patients.
New findings
New research at CIR has found that deleting the PTGER2 gene or blocking EP2 function amplifies reactivities of ILC2s, a type of immune cell that induce allergic immune responses in the lung. In contrast, forced activation of EP2 or EP4 (another protein that can also transduce PGE2’s biological actions) successfully represses allergic immune responses in the lung. Furthermore, PDE inhibitors, a medicine that has been approved for management or treatment of other conditions such as eczema, psoriasis, and chronic obstructive pulmonary disease, can also suppress lung allergic inflammation, sharing same downstream working mechanisms, i.e. through control of the immune cell ILC2 activities.
Therefore, this work not only shows how reduction of the lipid PGE2 and the protein EP2 is connected with NERD, but also implies that treatments that activate the EP2 and/or EP4 proteins can be beneficial for controlling lung allergies, asthma and NERD.
Scientists have long known that the PTGER2 gene changes in patients with NERD, but we have not previously understood why or what this means. Our study found that this gene alteration causes augmented lung allergic reactions, which suggests new strategies for controlling severe asthma and NERD.
This research project was funded by MRC UK and Cancer Research UK.
Find out more
Calum T Robb, You Zhou, Jennifer M Felton, Birong Zhang, Marie Goepp, Privjyot Jheeta, Danielle J Smyth, Rodger Duffin, Sonja Vermeren, Richard M Breyer, Shuh Narumiya, Henry J McSorley, Rick M Maizels, Jürgen K J Schwarze, Adriano G Rossi, Chengcan Yao (2022) Metabolic regulation by prostaglandin E2 impairs lung group 2 innate lymphoid cell responses. Allergy Online ahead of print.
PMID: 36181709
DOI: 10.1111/all.15541

