Whether born naturally or via cesarean section, babies receive essential microbes from their mothers
Do cesarean-born babies miss out on essential microbes? New evidence suggests that the answer may be “no.”
Researchers from the Centre for Inflammation Research and University Medical Center Utrecht report that mothers are able to transfer microbes to their babies via alternative, compensatory routes. While cesarean-born babies do receive less of their mother’s gut microbiome during birth, they make up for this by drinking their mother’s microbes in breastmilk.
Most microbiome research has focused on the gut, but people also house beneficial microbial communities in other parts of their bodies, such as in respiratory tracts and on skin. This study helps clarify how babies, who are generally considered microbiotically sterile before birth, get essential microbes for their various microbiomes.
We wanted to have a better idea of how the infant microbiome develops in different parts of their bodies and how it’s influenced by factors such as birth mode, antibiotic use, and lack of breastfeeding.
Collecting microbiome samples
To understand how the microbiome develops during the first month of life, the team recruited and repeatedly sampled 120 Dutch mothers and soon-to-be-born babies. From the babies, they collected skin, nose, saliva, and gut microbiome samples two hours after they were born and when they were one day old, one week old, two weeks old, and one month old.
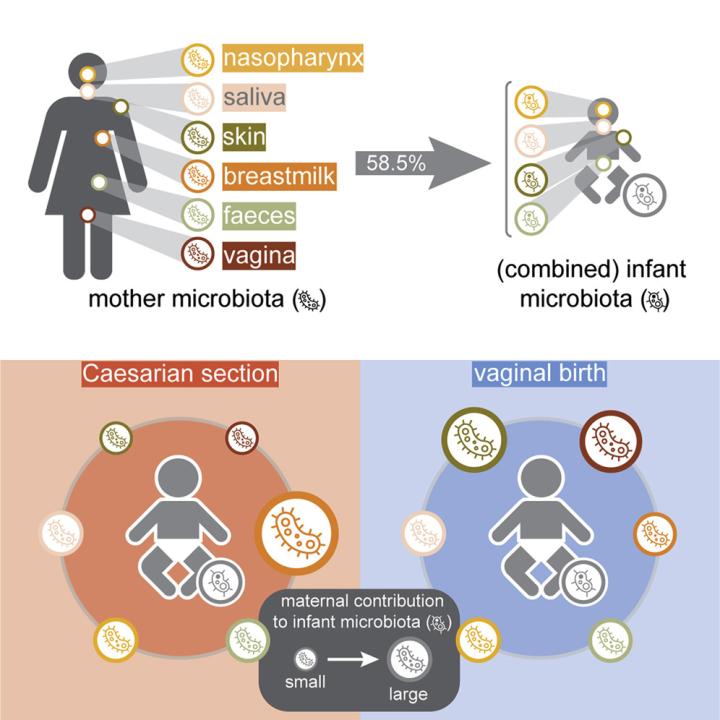
The team also collected six different types of microbiome samples from the mothers—skin, breastmilk, nose, throat, fecal, and vaginal—to determine which of these sources were “seeding” the babies’ various microbiomes. Then, they analyzed these results in the context of several factors that are thought to impact microbiome transfer, including mode of delivery, antibiotic use, and breastfeeding.
Key microbes use a variety of paths to reach infants
"We saw that many niches of the mother are important for the transmission of microbes, and if some of these pathways are blocked for one reason or another—in this case, we saw that happening with the cesarean section—then these microbes can still reach the infant through other paths," says Dr de Steenhuijsen Piters.
Regardless of birth route, the researchers found that approximately 58.5% of a baby’s microbiome is derived from its mother. However, different maternal microbial communities contributed to different infant microbiomes. Cesarean-born babies received fewer microbes from their mother’s vaginal and fecal microbiomes, but—seemingly in compensation—acquired more microbes from breastmilk.
Microbiome transfer and development are so important that evolution has ensured that those microbes are transferred one or another way from mother to child. Breastfeeding becomes even more important for children born by cesarean section who do not receive gut and vaginal microbes from their mom.
“It’s a smart system, and it makes sense from an evolutionary perspective that these types of pathways are redundant to ensure that the child can begin life with the appropriate ‘starter kit,’” says Dr de Steenhuijsen Piters.
Looking to the future
Now, the team want to know more about non-maternal influences on infant microbiome development. “We could see that the maternal microbiome explains almost 60% of the infant’s total microbiome, but there’s still 40% that we don't know about,” says Dr de Steenhuijsen Piters. “It would be interesting to stratify that unknown fraction to see where all the microbes come from; whether fathers contribute, for example, or siblings, or the environment.”
Ultimately, the researchers want to understand how microbiome development in infants relates to long-term health. “Next, we want to explore whether this early life process, influenced by mom, is affecting not only short-term infection risk in the first year of life but also longer-term health in terms of things like allergies and asthma,” says Professor Bogaert. “In the future, we might be able to utilize this knowledge to help prevent, diagnose, or treat health problems.”
This research was supported by the Netherlands Organisation for Scientific Research and the CSO/NRS through a Scottish Senior Clinical Fellowship award.
Cell Host and Microbe, Bogaert et al. “Mother-infant microbiota transmission and infant microbiota development across multiple body sites,” https://www.cell.com/cell-host-microbe/fulltext/S1931-3128(23)00043-4

