16 Sep 20. BJR Press release
BJR publishes special feature on imaging patients with stable chest pain.
BJR, the international research journal of the British Institute of Radiology, has published a collection of articles on the theme of imaging patients with stable chest pain, guest-edited by leading experts Professor Matthijs Oudkerk & Professor Edwin van Beek.
Millions of people around the world suffer from chest pain. Diagnosing the cause of chest pain & identifying the level of risk are integral to the prevention of serious coronary events & poor patient outcomes. Imaging is central to these efforts & provides vital information to primary care physicians, cardiologists & the variety of doctors who manage patients with stable chest pain.
Following the publication of the SCOT-HEART trial in 2015 (a study to see if coronary artery calcium score & computed tomography coronary angiogram alters the proportion of patients diagnosed with angina due to coronary heart disease), a new era of non-invasive coronary imaging has opened up. This BJR special feature covers many of the important topics & questions facing the scientists & clinicians working in the field & presents a collection of insightful Review articles & Commentaries from leading international experts.
Professor Edwin van Beek said “This special feature is essential reading for any medical professionals interested in stable chest pain. The articles cover vital topics such as vulnerable plaque, cost-effectiveness for imaging stable ischemic disease, the potential for functional coronary & cardiac CT imaging, the role of machine learning, the role of MRI for the assessment of chest pain & the role of imaging in the evaluation of heart valve disease”.
Professor Matthijs Oudkerk explains “This special feature marks the moment of publication of the first hard evidence that non-invasive coronary CT imaging in patients with chest pain saves lives compared to current medical practice & at the same time is a lot less harmful for the patient, costs less & is more effective. This special feature is not to be missed!”.
You can access the special feature, here.
Images
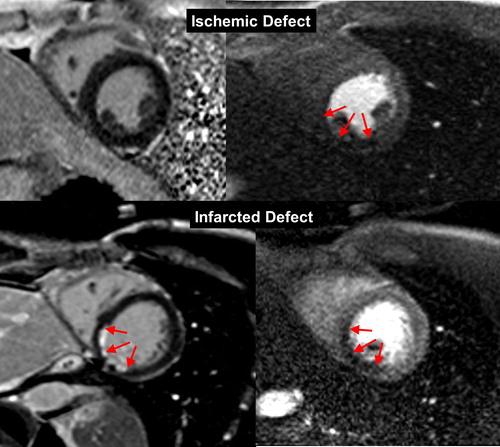
Figure 1 from "MRI perfusion in patients with stable chest-pain"
Figure 1. The top row is an example of an ischemic perfusion defect, where the stress perfusion image shows a clear hypoperfused area (red arrows), whereas the LGE image shows no defect.
The bottom row shows an infarct-related perfusion defect, where on both, stress perfusion (slightly hypoenhanced tissue, red arrows) and LGE image (strongly hyperenhanced tissue) a defect is shown (red arrows).
This example of an infarct patient also demonstrates the superiority of LGE to delineate scar in comparison to the perfusion approach.
In scar, the extracellular Gd-chelate contrast medium distributes in a large extracellular (fibrotic) compartment during first-pass, which increases the signal in the fibrotic tissue explaining its reduced sensitivity to detect hypoperfusion in scar.
This reduced sensitivity to detect hypoperfusion is not observed in viable myocardium (with small extracellular compartment). LGE, late gadolinium enhancement.

Figure 4. 18F-GP1 arterial uptake in right popliteal artery.
18F-GP1 PET-CT images of a patient who had recently undergone right common femoral artery endarterectomy & right popliteal artery angioplasty.
Anterior maximum intensity projection & axial images taken 120 min after 18F-GP1 injection show focal increased uptake in the right popliteal artery (a, b); arrows), which corresponds to a thrombotic lesion after angioplasty (c). Additional 18F-GP1 uptake is seen in the dissected right distal external iliac artery (d, e); dotted arrows) & right common femoral artery (a, f); arrow heads) where endarterectomy was performed 3 days prior to the PET-CT (g, arrow head).
Images courtesy of Chae et al.40 PET, positron emission tomography.
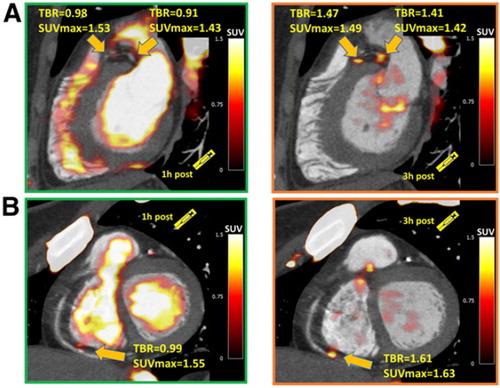
Figure 5 from "Vulnerable plaque imaging using 18F-sodium fluoride positron emission tomography"
Figure 5. Examples of coronary plaques with significant uptake on 3 h PET & low tracer activity of 1 h post injection imaging.
Short axis images of proximal left anterior descending, proximal circumflex (A) & distal right coronary artery (B) plaques (arrows) which had a TBR <1.0 on 1 h PET (left column) & showed uptake exceeding the 1.25 TBR threshold at 3 h.
This research was originally published in JNM. Kwiecinski J, Berman DS, Lee SE, Dey D, Cadet S, Lassen ML, Germano G, Jansen MA, Dweck MR, Newby DE, Chang HJ, Yun M, Slomka PJ. Three-Hour Delayed Imaging Improves Assessment of Coronary 18F-Sodium Fluoride PET. J Nucl Med. 2019 Apr;6025 :530–535. doi: 10.2967/jnumed.118.217885.
PET, positron emission tomography; SUV, standardized uptake value; TBR, target to background ratio.
Related links
- British Institute of Radiology
- British Journal of Radiology
- British Journal of Radiology special feature
- Professor Edwin van Beek
- Professor David Newby
- Professor Marc Dweck
- SCOT-HEART
- What is a CT scan?
- What is a PET scan?
- What is a MR scan?
- What is a PET-CT scan?
- "MRI perfusion in patients with stable chest-pain"
- "Non-invasive imaging of high-risk coronary plaque: the role of computed tomography & positron emission tomography"
- "Vulnerable plaque imaging using 18F-sodium fluoride positron emission tomography"
Social media tags & titles
BJR publishes special feature on imaging patients with stable chest pain. @BIR_News @BJR_Radiology @SINAPSECENTRE @MarcDweck #ChestPain

