Genes could be key to new Covid-19 treatments, study finds
Edinburgh researchers collaborating in the global GenOMICC consortium identify potential treatments for Covid-19 after the discovery of five genes associated with the most severe form of the disease: December 2020

Genetic evidence is second only to clinical trials as a way to tell which treatments will be effective against a disease. Existing drugs that target the actions of the genes reveal which drugs should be repurposed to treat Covid-19 in clinical trials, experts say.
Genes involved in two molecular processes - antiviral immunity and lung inflammation - were pinpointed. The breakthrough will help doctors understand how Covid-19 damages lungs at a molecular level.
Scientists from the University of Edinburgh - led by the Roslin Institute and including researchers from the MRC Human Genetics Unit, Centre for Genomic and Experimental Medicine and Edinburgh Clinical Research Facility - made the discovery by studying the DNA of 2,700 patients in 208 intensive care units (ICU) across the UK.
Researchers from the GenOMICC consortium – a global collaboration to study genetics in critical illness – compared the genetic information of Covid-19 patients in ICU with samples provided by healthy volunteers from other studies, such as UK Biobank, Generation Scotland and 100,000 Genomes.
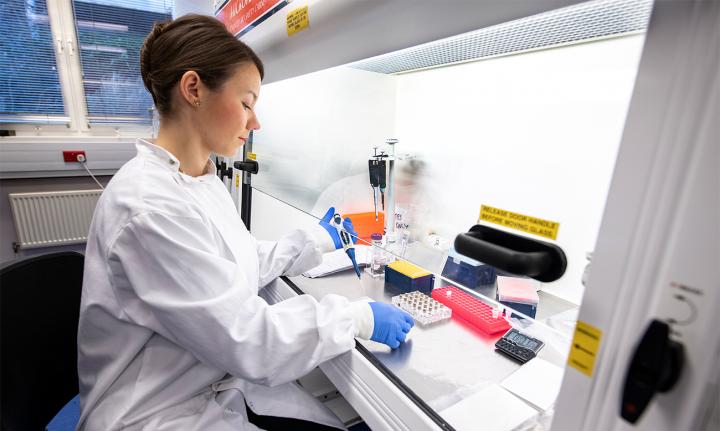
Blood samples were received by the Edinburgh Clinical Research Facility where they were expertly stored and their DNA extracted and genotyped. With support from the Bioinformatics Analysis Core at IGMM, the team used sophisticated statistical and computational tools to identify differences in the genetic code of patients and healthy volunteers.
The team found key differences in five genes of the ICU patients compared with samples provided by healthy volunteers. The genes - IFNAR2, TYK2, OAS1, DPP9 and CCR2 – partially explain why some people become desperately sick with Covid-19, while others are not affected.
Having highlighted the genes, the team were then able to predict the effect of drug treatments on patients, because some genetic variants respond in similar ways to particular drugs.
For example, they showed that a reduction in the activity of the TYK2 gene protects against Covid-19. An existing class of anti-inflammatory drugs called JAK inhibitors lowers TYK2 activity. One drug in this class, baricitinib, is approved for treatment of rheumatoid arthritis.
They also discovered that a boost in the activity of the gene INFAR2 is also likely to create protection, because it is likely to mimic the effect of treatment with interferon - proteins released by cells of the immune system to defend against viruses. However, experts caution that to be effective, patients might need the treatment early in disease.
Based on the findings published in Nature, the researchers say that clinical trials should focus on drugs that target these specific antiviral and anti-inflammatory pathways.
This is a stunning realisation of the promise of human genetics to help understand critical illness. Just like in sepsis and influenza, in Covid-19, damage to the lungs is caused by our own immune system, rather than the virus itself. Our genetic results provide a roadmap through the complexity of immune signals, showing the route to key drug targets. Our results immediately highlight which drugs should be at the top of the list for clinical testing. We can only test a few drugs at a time, so making the right choices will save thousands of lives. This work is only possible because of the generous contribution of the patients themselves and their families, research teams in NHS hospitals across the country, and the generous funding we’ve received from the public and organisations.
This study shows the power of genetics to inform medical decisions. Working within such a multi-disciplinary team to fight Covid-19 has been a privilege. We now hope that further understanding on Covid-19 will come from studying the genetics of symptom duration and how symptoms change over time in non-hospitalised patients. For this, it is vital that those that have or have had Covid-19 everywhere in the world join studies such as our parallel study Coronagenes.
Managing, cleaning, and processing massive sets of genetic and clinical data is key to rapid analysis for time critical projects such as this. We’ve been proud to contribute our expertise in this area to the GenOMICC consortium, and will continue working to build high quality datasets that can be analysed for direct impact on Covid-19 healthcare.