Peter Hall
Clinical Informatics and Health Economics in Cancer

Research in a Nutshell
Professor Peter Hall is an academic Medical Oncologist with a research interest in Health Economics and Health Technology Assessment in Cancer.
The focus of his research is on the development of improved methods for efficient research design, cost-effectiveness analysis and the measurement of clinical and socioeconomic outcomes using data obtained from research and routinely collected within the NHS.
He is Chief Investigator, clinical Co-Investigator or lead Health Economist on a number of clinical trials and methodological research projects. He leads the Health Economics Group within the University of Edinburgh Clinical Trials Unit. He is a Visiting Associate Professor of Health Economics at the Academic Unit of Health Economics, University of Leeds where he completed a PhD in health economic modelling. He is a NICE Appraisal Committee member and advises the Innovative Healthcare Delivery Programme Scotland. He treats patients with breast cancer at the Edinburgh Cancer Centre.
People |
|
| Peter S Hall | Principal Investigator, Professor of Cancer Informatics and Consultant Medical Oncologist |
|
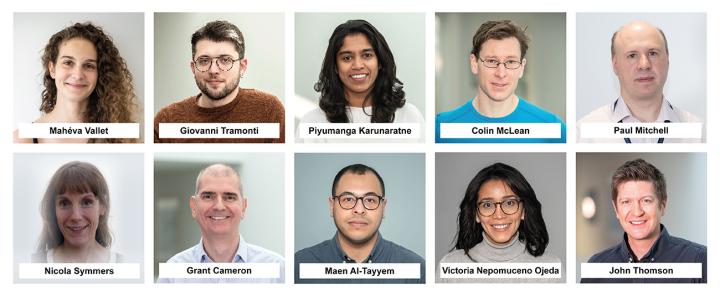
Mahéva Vallet |
Senior Research Manager |
| Giovanni Tramonti | Research Fellow |
| Piyumanga Karunaratne | Research Assistant |
| Colin McLean | Senior Data Scientist |
| Paul Mitchell | Developer |
| Nicola Symmers | Developer |
| Grant Cameron | Data Manager |
| Maen Al-Tayyem | Clinical Research Coder |
| Victoria Nepomuceno Ojeda | Clinical Research Coder |
| John Thomson | Senior Bioninformatician |
Contact
Collaborations
- DATA-CAN (the health data research hub for cancer)
- NIHR Diagnostic Evidence Cooperative
- Precision Medicine Catapult
- National Institute for Care Excellence (NICE)
- NCRI Psychosocial and Survivorship Clinical Studies Group
- EORTC
- Scottish Medicines Consortium
- Scottish Molecular Pathology Evaluation Panel
- Edinburgh-St Andrews MRC Molecular Pathology Node
- Farr Institute
- Canadian Paceomics Programme
Partners and Funders
- 2013–2022 NIHR (Health Technology Assessment), £2 million “Mammographic surveillance in breast cancer patients aged over 50 years” Mammo-50: A multi-centre, randomised, controlled, phase III trial of annual mammography versus 2 yearly for conservation surgery patients and 3 yearly for mastectomy patients.
- 2012–2019 Cancer Research UK (CTAAC), £500,000 Chemotherapy options for frail and elderly patients with advanced gastro-esophageal cancer: A UK Randomised controlled trial. (GO-2)
- 2013 – 2017 NIHR Diagnostics Evidence Co-operative £1m (Leeds – Cancer, Renal, Musculoskeletal and Liver diseases).
- 2013-16 Technology Strategy Board Small Business Research Initiative £1.8m, Development of a home monitoring device for neutropenia. Collaborator, in collaboration with Phillips.
- 2013-14 Technology Strategy Board Small Business Research Initiative £347,000, Detection and Identification of infectious agents: Assessing the impact of near patient testing. Network Tools for Intervention Modelling In Sepsis. Collaborator, in collaboration with X-Lab Systems Ltd.
- 2014-2016 NIHR Health Technology Assessment £176,842. The future for diagnostic tests for acute kidney injury in critical care: Evidence synthesis, care pathway analysis and research prioritisation “AKI-Diagnostics”
- 2014-2016 NIHR Research for Patient Benefit. In collaboration with the Christie Clinical Trials Unit). Randomised controlled trial of acupuncture plus standard care versus standard care for chemotherapy induced peripheral neuropathy (CIPN). “ACUFOCIN”
- 2014-2017 NIHR Research for Patient Benefit £250,000. A study to determine the feasibility and acceptability of conducting a phase III randomised controlled trial comparing stereotactic Ablative Radiotherapy (SABR) with surgery in patients with peripheral stage I non-small cell lung cancer (NSCLC) considered to be at higher risk of complications from surgical resection. “SABRTOOTH”
- 2015-2018 MacMillan research grant £565,849. In collaboration with the University of Leeds. The use of comprehensive patient records (CPR) to define the impact of cancer, co-morbidities and late effects on individuals and the health service.
- 2015-2017 NHS England Research Innovation fund, £200,000 In partnership with Caris Life Sciences International. Pilot study to assess feasibility of tumour profiling for solid tumour cancer patients in the NHS.
- 2015 – 2020 Yorkshire Cancer Research. £1.5m A randomised controlled trial of the effect of the omega-3 fatty acid eicosapentaenoic acid (EPA) on survival after liver resection surgery for colorectal cancer metastasis (The EMT2 study).
- 2016-2017 Innovate UK SBRI. T-cell receptor diversity evaluation as a predictive biomarker of response to immunotherapy (In collaboration with ImmunID).
Scientific Themes
Clinical Informatics, Health Economics, Cancer, Real-world data
Technology Expertise
Decision Analysis, Cost Analysis, Cost-effectiveness Analysis, Clinical Trials Design, Efficient Research Design